# 5362
By just about any standard, we dodged a bullet with the pandemic of 2009. Despite hundreds of thousands of hospitalizations and tens of thousands of deaths (far more than were officially counted), it could have been far worse.
But we may not be out of the woods just yet.
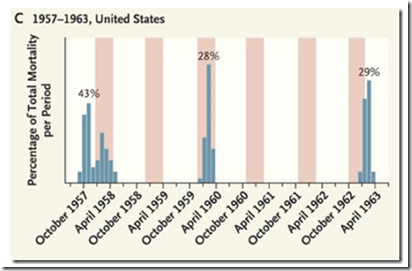
It isn’t lost on scientists that in 1957, the Asian Flu pandemic seemed to disappear completely for more than a year, only to return in 1959 and again after a two year lull during the 1962-63 flu season.
Influenza viruses are – as we’ve said before – unpredictable.
Two things we look for in an emerging virus are its pathogenicity – its ability to cause disease, and its transmissibility in humans – often measured by its R0 (pronounced `R nought’) or basic reproductive number.
This R0 number describes the average number of new cases caused by one infectious person entering a totally susceptible population If less than 1.0, outbreaks are likely to sputter and die out.
With an R0 greater than 1.0, an outbreak has `legs’, and can spread through a community.
Determining the R0 of a virus can only be done in retrospect, and that number may vary considerably from one community to another. The best researchers can usually come up with is an estimated range.
For the 2009 H1N1 virus, that number has usually been pegged at between 1.4 and 1.6. Fairly low for a pandemic virus, but sufficient to ensure its survival and spread.
The 1918 pandemic virus, in comparison, has been estimated to have an R0 between 2.0 and 3.0. There are some estimates that run even higher.
In order to spread efficiently, a virus must be able to bind to human receptor cells – preferably those found in the upper airway. While H1N1 does bind to human α2,6 receptor cells, it appears to do so more weakly than do many other flu viruses.
Additionally, in 2009 researchers at MIT and the CDC found that a portion of the PB2 gene – which is normally found in efficiently transmitted influenza viruses – was missing.
From MIT News, July 3rd 2009.
MIT, CDC find H1N1 flu virus ill-suited for rapid transmission
But researchers say new strain bears watching, could mutate
(EXCERPT)
Recent studies have shown that a viral RNA polymerase known as PB2 is critical for efficient influenza transmissibility. (RNA polymerase controls the viruses' replication once they infect a host.) The new H1N1 strain does not have the version of the PB2 gene necessary for efficient transmission.
While we’ve been relatively fortunate so far, the question becomes, what would it take to make the 2009 pandemic virus more dangerous?
While there is probably more than one answer to that question, once again researchers from MIT and the CDC have been investigating, and have recently presented the results of a laboratory generated single point mutation that confers enhanced transmissibility to the H1N1 virus (at least in ferrets).
Ferrets are often used in influenza studies because their respiratory physiology, and susceptibility to influenza viruses, is close to that of humans.
The study, which appears in the March 2nd edition of Plos One, is called:
A Single Base-Pair Change in 2009 H1N1 Hemagglutinin Increases Human Receptor Affinity and Leads to Efficient Airborne Viral Transmission in Ferrets
Akila Jayaraman, Claudia Pappas, Rahul Raman, Jessica A. Belser, Karthik Viswanathan, Zachary Shriver, Terrence M. Tumpey, Ram Sasisekharan
The 2009 H1N1 influenza A virus continues to circulate among the human population as the predominant H1N1 subtype. Epidemiological studies and airborne transmission studies using the ferret model have shown that the transmission efficiency of 2009 H1N1 viruses is lower than that of previous seasonal strains and the 1918 pandemic H1N1 strain.
We recently correlated this reduced transmission efficiency to the lower binding affinity of the 2009 H1N1 hemagglutinin (HA) to α2→6 sialylated glycan receptors (human receptors). Here we report that a single point mutation (Ile219→Lys; a base pair change) in the glycan receptor-binding site (RBS) of a representative 2009 H1N1 influenza A virus, A/California/04/09 or CA04/09, quantitatively increases its human receptor-binding affinity.
The increased human receptor-affinity is in the same range as that of the HA from highly transmissible seasonal and 1918 pandemic H1N1 viruses. Moreover, a 2009 H1N1 virus carrying this mutation in the RBS (generated using reverse genetics) transmits efficiently in ferrets by respiratory droplets thereby reestablishing our previously observed correlation between human receptor-binding affinity and transmission efficiency. These findings are significant in the context of monitoring the evolution of the currently circulating 2009 H1N1 viruses.
For a less technical take on all of this, MIT News has an article describing the ramifications of this discovery.
Keeping an eye on H1N1
MIT scientists identify a mutation that could allow the flu virus to spread much more easily.
Despite all of our technology, and an unprecedented two-year focus on the 2009 H1N1 virus, scientists are just beginning to unravel the secrets of the internal workings of flu viruses.
We can readily observe changes to the virus’s structure, but only rarely can we predict what those changes may mean in terms of virulence or transmissibility.
We know, for instance, that the H275Y mutation confers oseltamivir resistance, and although we’ve been watching the D225G `Norway’ mutations around the globe for more than a year, the jury is still out on its clinical significance (see Eurosurveillance: Debating The D222G/N Mutation In H1N1).
It isn’t enough to simply observe mutations occurring in the influenza virus.
We need to know that they mean.
To that end, this research has identified a potentially dangerous single point mutation that – should it begin appearing in the wild – could signal the start of a new wave of illness.
While that may not happen with the 2009 H1N1 virus, knowing what to look for gives us a decided advantage when tracking the evolution of this – and any other – influenza virus.