Thermal Scanner – Credit Wikipedia
# 6593
While there are no indications that the coronavirus detected recently in the Middle East has spread beyond the first two cases, some places around the world are taking this threat very seriously.
For example, local media is reporting that thermal scanners have been deployed at the Ninoy Aquino International Airport in the Philippines in an attempt to screen arrivals from the Middle East for possible infection.
Whenever a novel virus appears, people’s thoughts understandably turn to a pandemic scenario, even though experience has shown that most emerging viruses don’t have the `legs’ to spark a global epidemic (see Novel Viruses & Chekhov’s Gun).
Nevertheless, history tells us that pandemics come along several times each century, and another pandemic is all but inevitable.
And so the world’s attention this week has quite naturally focused on the novel coronavirus that killed one man in Saudi Arabia last July and has a Qatari man currently hospitalized in London.
Memories of the SARS outbreak in 2002 and 2003 remain vivid, particularly in Asia, where the virus hit hardest.
Fortunately, while there is still much we don’t know about this emerging pathogen, there are no immediate signs that this virus poses a pandemic threat.
While we may not know when - or which virus - will spark the next global health crisis, we have pretty good idea how it will arrive in most countries.
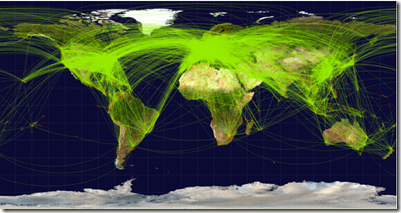
Scheduled airline traffic around the world, circa June 2009 – Credit Wikipedia
The world’s airlines carry 2.6 billion passengers each year, on more than 17 million flights. And as the map above indicates, millions of them are international flights.
With most viral diseases having an incubation period of several days or longer, someone who is newly infected with a virus could change planes and continents several times before showing their first signs of illness.
Last July, in MIT: Contagion Dynamics Of International Air Travel we looked at a study appearing in PloS One, that simulated the early spread of a pandemic virus via air travel and ranked U.S. airports based on how much they contributed to the spread of the illness.
An excerpt from a report that appeared in MIT News.
New model of disease contagion ranks U.S. airports in terms of their spreading influence
Airports in New York, Los Angeles and Honolulu are judged likeliest to play a significant role in the growth of a pandemic.
Kennedy Airport is ranked first by the model, followed by airports in Los Angeles, Honolulu, San Francisco, Newark, Chicago (O'Hare) and Washington (Dulles). Atlanta's Hartsfield-Jackson International Airport, which is first in number of flights, ranks eighth in contagion influence. Boston's Logan International Airport ranks 15th.
All of which begs the question, can we really screen, identify, and isolate infectious airline passengers before they can spread a pandemic virus?
Sadly, the evidence to date has not been very encouraging.
Last April, in EID Journal: Airport Screening For Pandemic Flu In New Zealand, we examined a study that found the screening methods used at New Zealand’s airport were inadequate to slow the entry of the 2009 pandemic flu into their country, detecting less than 6% of those infected.
New Zealand did not employ thermal scanners, although countries that did, didn’t fare much better.
Proving that `there’s no place like home’ during a global crisis, in Vietnam Discovers Passengers Beating Thermal Scanners, we saw evidence of passengers taking fever-reducers to beat the airport scanners in a desperate attempt to get home.
In December of 2009, in Travel-Associated H1N1 Influenza in Singapore, I blogged on a NEJM Journal Watch article on of a new study that has been published, ahead of print, in the CDC’s EID Journal entitled:
Epidemiology of travel-associated pandemic (H1N1) 2009 infection in 116 patients, Singapore. Emerg Infect Dis 2010 Jan; [e-pub ahead of print]. Mukherjee P et al
Travel-Associated H1N1 Influenza in Singapore
Airport thermal scanners detected only 12% of travel-associated flu cases; many travelers boarded flights despite symptoms.
In June of 2010 CIDRAP carried this piece on a study of thermal scanners in New Zealand in 2008 (before the pandemic) presented at 2010’s ICEID.
Thermal scanners are poor flu predictors
Thermal scanners for screening travelers do moderately well at detecting fever, but do a poor job at flagging influenza, according to researchers from New Zealand who presented their findings today at the International Conference on Emerging Infectious Diseases (ICEID) in Atlanta.
And in early 2009, Helen Branswell penned an article for the Canadian Press, that stated:
Studies show little merit in airport temperature screening for disease
Monday, 16 February 2009 - 11:58am.
By Helen Branswell
TORONTO — Using temperature scanners in airports to try to identify and block entry of sick travellers during a disease outbreak is unlikely to achieve the desired goal, a report by French public health officials suggests.
The evidence is pretty clear.
With the technology of today, coupled with likelihood of having many pre-symptomatic and asymptomatic carriers, there isn’t much hope to identify more than a fraction of infected travelers.
As far as the risk of catching a pandemic flu virus while a passenger on an airliner, in May of 2010 we saw a study that appeared in the BMJ that looked at that very topic (see BMJ: Flu Transmission Risks On Airplanes)
BMJ 2010;340:c2424
Research
Transmission of pandemic A/H1N1 2009 influenza on passenger aircraft: retrospective cohort study
Conclusions
A low but measurable risk of transmission of pandemic A/H1N1 exists during modern commercial air travel. This risk is concentrated close to infected passengers with symptoms. Follow-up and screening of exposed passengers is slow and difficult once they have left the airport.
Another study, conducted by researchers at UCLA and published in BMC Medicine in late 2009:
Calculating the potential for within-flight transmission of influenza A (H1N1)
Bradley G Wagner, Brian J Coburn and Sally Blower*
Results
The risk of catching H1N1 will essentially be confined to passengers travelling in the same cabin as the source case. Not surprisingly, we find that the longer the flight the greater the number of infections that can be expected. We calculate that H1N1, even during long flights, poses a low to moderate within-flight transmission risk if the source case travels First Class.
While there will likely be intense public clamor to try to block the entry of a pandemic virus into this, or any other country, the truth is – it is highly unlikely that it will work.
Areas that receive a very small number of arrivals might be able to institute a quarantine system (see Can Island Nations Effectively Quarantine Against Pandemic Flu? ), but even then the ability to identify and isolate infected travelers won’t be 100%.
Still, even if the success rate is likely to be low, there may be some value in trying to limit the number of infected persons arriving into a country, particularly during the opening days and weeks of an outbreak.
The more introductions of a virus into a population, the more points it will have from which to spread.
Since it takes months to produce and deploy a vaccine, and time to prepare a society to deal with a pandemic, any delaying action that can reduce the speed and spread of the virus has value.
The takeaway from all of this is that we ignore global healthcare and infectious disease outbreaks – even in the remotest areas of the world – at our own peril.
Vast oceans and extended travel times no longer offer us protection, and there is no technological shield that we can erect that would keep an emerging pandemic virus out.
The place to try to stop the next pandemic is not at the gate, but in the places around the world where they are likely to emerge.
Which makes the funding and support of international public health initiatives, animal health initiatives, and disease surveillance ever so important, no matter where on this globe you happen to live.