#14,132
Three summers ago (June 24th, 2016) the CDC issued a Clinical Alert to U.S. Healthcare facilities about the Global Emergence of Invasive Infections Caused by the Multidrug-Resistant Yeast Candida auris.
C. auris is an emerging fungal pathogen that was first isolated in Japan in 2009. It was initially found in the discharge from a patient's external ear (hence the name `auris'). Retrospective analysis has traced this fungal infection back over 20 years.A week later we saw a release from the UK's PHE On The Emergence Of Candida auris In The UK, where they detailed a large (and ongoing since April 2015) nosocomial outbreak at an adult critical care unit in England.
Since then we've been following the progress of this emerging pathogen - both in the United States and around the world - because:
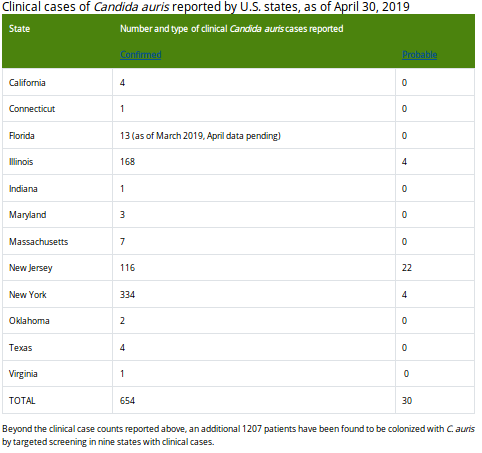
Late this week the CDC published their June update on their C. Auris surveillance page, where they show - as of April 30th - 654 confirmed cases and 30 probable cases, across 12 states (primarily New York, New Jersey & Illinois).
- C. auris infections have a high fatality rate
- The strain appears to be resistant to multiple classes of anti-fungals
- This strain is unusually persistent on fomites in healthcare environments.
- And it can be difficult for labs to differentiate it from other Candida strains
Additionally, 1207 patients have been found to be asymptomatically colonized with C. auris through targeted screening conducted in six states with clinical cases.To put this into perspective, this represents a roughly 25% increase in cases since the EOY 2018 numbers (520 confirmed), in just the first four months of 2019. First some excerpts from the latest CDC update, followed by a couple of recently published articles and/or studies.
Tracking Candida auris
June 14, 2019: Case Count Updated as of April 30, 2019
U.S. Map
World Map
Candida auris is an emerging fungus that presents a serious global health threat. C. auris causes severe illness in hospitalized patients in several countries, including the United States. Patients can remain colonized with C. auris for a long time and C. auris can persist on surfaces in healthcare environments. This can result in spread of C. auris between patients in healthcare facilities.
Most C. auris cases in the United States have been detected in the New York City area, New Jersey, and the Chicago area. Strains of C. auris in the United States have been linked to other parts of the world. U.S. C. auris cases are a result of inadvertent introduction into the United States from a patient who recently received healthcare in a country where C. auris has been reported or a result of local spread after such an introduction.
Candida auris was made nationally notifiable at the 2018 Council for State and Territorial Epidemiologists (CSTE) Annual Conference. For the updated case definition and information on the nationally notifiable condition status, please see the 2018 CSTE position statement pdf icon[PDF – 16 pages].
CDC encourages all U.S. laboratories that identify C. auris to notify their state or local public health authorities and CDC at candidaauris@cdc.gov. CDC is working closely with public health and healthcare partners to prevent and respond to C. auris infections. The CDC-sponsored Antibiotic Resistance Laboratory Network (ARLN) will help improve detection and response to C. auris nationwide.(Continue . . . )
Our next stop is the AJIC (American Journal of Infection Control) whose June issue carries an analysis of early cases detected in New York State.
American Journal of Infection Control
Volume 47, Issue 6, Supplement, June 2019, Page S10
Presentation Number OIPH-21A
Description of the First Candida Auris-colonized Individuals in New York State, 2016-2017
https://doi.org/10.1016/j.ajic.2019.04.155
(EXCERPT)
RESULTS
Between 10/5/2016 and 11/7/2017, 114 facility-based surveillance cases were identified. The median age was 74 years (range 23-100 years). Facility-based surveillance cases had a median of three HCF admissions in 90 days before first positive culture (range 0-8). Ninety-three percent were from facilities in Brooklyn or Queens. Fifty-four percent had diabetes.
During the week before first positive culture, 81% received mechanical ventilation, 80% had tracheostomy, and 70% had a percutaneous feeding tube. Thirty-four percent had no prior indications for Contact Precautions at time of first positive culture. To date only 9% had serial negative C. auris surveillance cultures. Sixty-two percent were known to be deceased.(Continue . . . . )
We also get this overview overview from the Miami-Dade Florida Department of Health's March Epi Monthly report (excerpts below).
Candida auris: An Emerging Global Health Threat
By: Sebastian Arenas
Introduction
Candida auris is an emerging fungus that presents a serious global health threat. The concern is based on three main reasons: multidrug resistance, frequent misidentification, and potential to cause outbreaks in health care settings.
C. auris was first isolated in Japan and described as a new species in 2009. Subsequently, it was later isolated from patients in South Korea, Kuwait, South Africa, and Venezuela. Cases in the United States are a result of introduction by patients with international health care exposures where C. auris has been reported or as a result of local spread after such an introduction.
Most cases in the U.S. have been detected in recent years in New York, Illinois, and New Jersey with a total of 561 confirmed cases. As of March 29, 2019, Florida has 12 confirmed cases based on the latest tracking data from the Centers for Disease Control and Prevention (CDC). 1
How Serious is C. auris?
C. auris has been isolated most frequently from hospitalized patients and can be fatal; more than 1 in 3 patients with invasive C. auris infections die. 2 The patients with the highest risk for colonization and/or infection are those with prolonged hospitalizations, tracheostomy and ventilator dependence, intensive care unit admissions, indwelling devices (e.g., central lines, peg tubes), recent surgeries, and immunosuppression. 3
Furthermore, C. auris has demonstrated multidrug resistance properties worldwide, which has not been seen in other Candida species. 3 Most infections are treatable with a class of antifungal drugs called echinocandins.
However, some C. auris infections have been resistant to all three main classes of antifungal medications, making them more difficult to treat. 4 In addition, C. auris can be misidentified as a number of different organisms when using identification methods such as VITEK 2 YST, API 20C, BD Phoenix yeast identification system, and MicroScan. 5
An increase in unidentified Candida infections in a patient care unit should raise suspicion for C. auris because of its ability to cause nosocomial outbreaks.(Continue . . . )
And finally, some on-topic studies we've looked at previously include:
Candida auris in Healthcare Facilities, New York, USA, 2013–2017
Candida auris in South Africa, 2012–2016
Emerging Fungal Pathogen Candida auris Evades Neutrophil Attack
And some past blogs include:
Notes from the Field: Surveillance for Candida auris — Colombia, September 2016–May 2017)
ECDC: C. Auris Rapid Risk Assessment For Healthcare Settings - Europe
mSphere: Comparative Pathogenicity of UK Isolates of the Emerging Candida auris