# 4072
Yesterday one of my readers left this question in the comments section of ECDC On Norway Mutation & Tamiflu Resistance.
h1n1_watcher said...
regarding the concern about mutations there is one thing I don't understand: If influenza viruses are constantly changing by genetic drift anyway, then why has this never led to a more dangerous form of the seasonal influenza during all those years and decades of constant genetic drift. i.e. ongoing mutation ?
The pathogenicity/CFR or virulence of seasonal influenza seems to be almost exactly the same every year for decades despite the fact that the virus is constantly mutating.
Why is this so ? and why is a pandemic virus supposed to be more prone to "dangerous" mutations than the seasonal ones ?
As far as I know the mutation (drift) rates are similar for both seasonal and pandemic viruses. Yet is has never been observed that a seasonal influenza virus has mutated to a more deadlier form. (Usually, the only consequence of the mutations is that we have to update our vaccines accordingly ...)
h1n1_Watcher has posed some intriguing questions, and while I don’t have all of the answers, I’d like to take a stab at part of it.
While several points are raised, the recurring central issue is:
If influenza viruses are constantly changing by genetic drift anyway, then why has this never led to a more dangerous form of the seasonal influenza during all those years and decades of constant genetic drift. i.e. ongoing mutation ?
The problem here is, I don’t think we can make this assumption.
There have been great variations documented in the virulence (and transmissibility) of seasonal influenza viruses from one year to the next.
The CDC statement that influenza kills 36,000 Americans every year is a bit misleading, because the death toll between 1990 and 1999 from which that estimate arose was calculated to range from a low of 17,000 to a high of 52,000.
And none of those were `pandemic years’.
Some of this variation can be attributed to years when the more virulent H3N2 virus was the dominant strain, as opposed to the milder H1 strain, but we’ve seen year-to-year variations in the virulence of the same seasonal virus.
I’m going to be drawing a good deal of material from an absolutely fascinating EID Journal article: Viboud C, Tam T, Fleming D, Miller MA, Simonsen L. 1951 influenza epidemic, England and Wales, Canada, and the United States.
Abstract (Excerpt)
Influenza is responsible for large increases in deaths in pandemic seasons when emerging viral subtypes with novel surface antigens become predominant, and also in some interpandemic seasons, when established subtypes exhibit antigenic drift (1).
The circulating viral subtype is associated with varying severity of influenza epidemics (2): in the last 2 decades in the United States, estimated excess death rates were on average 2.8-fold higher in A/H3N2-dominated seasons than in A/H1N1 and B seasons (3).
Within a given subtype, however, the strain-specific determinants of epidemic severity are still poorly understood. For instance in the United States in the same period, excess death rates varied nearly 4-fold among A/H3N2 seasons, even after adjustments for population aging (3).
So, even over the past quarter century, we’ve seen major differences in the virulence of the same seasonal flu strain.
The most telling example, however, came in 1950-51.
The no-name epidemic of 1951 was one that, for a few weeks - mostly in England and Canada- proved to be deadlier than the 1918 Spanish Flu.
For most of the world, 1951 remained an average flu year. The dominate strain of influenza that year was the so-called `Scandinavian strain', which produced mild illness in most of its victims.
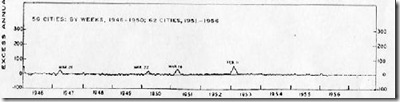
In fact, if you look at the graph for the United States, running from 1945 to 1956, you'll see nary a blip.
But in December of 1950 a new strain of virulent influenza appeared in Liverpool, England, and by the end of the flu season, had spread across much of England, Wales, and Canada.
Again, from the EID Study.
The 1951 influenza epidemic (A/H1N1) caused an unusually high death toll in England; in particular, weekly deaths in Liverpool even surpassed those of the 1918 pandemic. . . . . Why this epidemic was so severe in some areas but not others remains unknown and highlights major gaps in our understanding of interpandemic influenza.
According to this study, the effects on the city of origin, Liverpool, were horrendous.
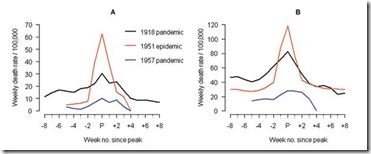
In Liverpool, where the epidemic was said to originate, it was "the cause of the highest weekly death toll, apart from aerial bombardment, in the city's vital statistics records, since the great cholera epidemic of 1849" (5). This weekly death toll even surpassed that of the 1918 influenza pandemic (Figure 1)
This extraordinary graph shows the excess deaths in Liverpool during this outbreak (red line), while the black line shows the peak deaths during the 1918 pandemic. This chart shows excess deaths by A) respiratory causes (pneumonia, influenza and bronchitis) and B) all causes.
For roughly 5 weeks Liverpool saw an incredible spike in deaths due to this new influenza. And it did not remain just in Liverpool. While it appears not to have spread as easily as the dominant Scandinavian strain, it managed to infect large areas of England, Wales, and Canada over the ensuing months.
For reasons we don't understand, this new strain never managed to spread much beyond England, Wales, and Canada. It did not reappear the next flu season either. It vanished as mysteriously as it appeared.
Another example, but one that affected the transmissibility and not the virulence of the seasonal virus, occurred in 1947. The so-called `vaccine failure’ year, when a new H1N1 virus swept quickly around the world.
In what would later be described as the Pseudopandemic of 1947, a new variant of the H1N1 appeared on military bases – first noticed in Japan – and quickly spread from there. While it produced a generally mild illness (sound familiar?) there were apparently low levels of immunity in the population.
1947 is little remembered today, except by epidemiologists, because while widespread, this new flu strain produced few excess deaths.
While we tend to worry about mutations and antigenic changes to pandemic strains, the truth is, plain old seasonal influenza is quite capable of throwing us a curveball.
It has in the past, and no doubt will do so again in the future.
My thanks for the question, and an opportunity to revisit one of my favorite influenza research papers. Hopefully this answers at least part of the reader’s question.