Photo Credit – CDC
# 7252
While we await the next installment in the nCoV and H7N9 story, we’ve a new study that appeared yesterday in JAMA Psychiatry, that links bipolar disorder (BD) to influenza exposure while still in the womb.
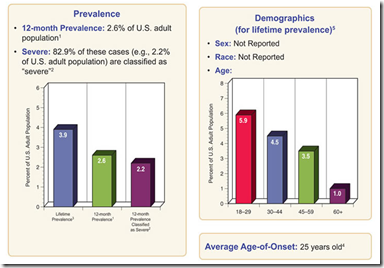
Some background information on BD from the NIMH, that shows millions of Americans suffer to one degree or another from this disorder.
Bipolar Disorder Among Adults
Bipolar disorder, sometimes referred to as manic-depressive disorder, is characterized by dramatic shifts in mood, energy, and activity levels that affect a person’s ability to carry out day-to-day tasks. These shifts in mood and energy levels are more severe than the normal ups and downs that are experienced by everyone.
Additional information about bipolar disorder can be found on NIMH’s bipolar disorder page.
As you might imagine, it takes the review of decades of health data to link a viral exposure in the womb to the development of any adult-onset illness.
And that’s exactly what researchers from Columbia University Medical Center, the New York State Psychiatric Institute, Kaiser Permanente, in Oakland, California; and the University of KwaZulu-Natal Durban, South Africa did.
Using data derived from Kaiser Permanente Health Plan's Northern California region, researchers checked for influenza diagnoses among pregnant women enrolled between 1959 and 1966, and then followed up on their offspring’s medical records for diagnoses consistent with bipolar disorder later in life.
Based on a relatively small, and geographically limited data set, researchers found a nearly 4-fold increase (3.82 times) in bipolar disorder among offspring whose mother had experienced an influenza infection during pregnancy, compared to offspring not exposed to the virus as a fetus.
First a link to the study (and some excerpts from the abstract), then I’ll return with more.
Gestational Influenza and Bipolar Disorder in Adult Offspring
Raveen Parboosing, MBChB, MMed, FCPath(SA)(Viro), MS; Yuanyuan Bao, MS; Ling Shen, PhD; Catherine A. Schaefer, PhD; Alan S. Brown, MD, MPH
JAMA Psychiatry. 2013;():1-8. doi:10.1001/jamapsychiatry.2013.896.
(EXCERPT)
Main Outcome and Measures Bipolar I or II disorder, BD not otherwise specified, or BD with psychotic features.
Results We found a significant, nearly 4-fold increase in the risk of BD (odds ratio, 3.82 [95% CI, 1.58-9.24; P = .003]) after exposure to maternal influenza at any time during pregnancy. The findings were not confounded by maternal age, race, educational level, gestational age at birth, and maternal psychiatric disorders.
Conclusions and Relevance Maternal influenza may be a risk factor for BD. Although replication is required, the findings suggest that prevention of maternal influenza during pregnancy may reduce the risk of BD.
As with all observational studies, there are some weaknesses that must be considered, including: the relatively small cohort of patients studied, the lack of lab confirmation of maternal flu diagnosis, and difficulties in finding intact medical histories on offspring.
That said, over the past decade we’ve seen a growing number of studies that have tentatively linked prenatal exposure to influenza (or an influenza-like-illness) to a variety of child, adolescent, and adult psychiatric and developmental disorders.
A few examples include:
- In a 2004 study (Serologic evidence of prenatal influenza in the etiology of schizophrenia Brown et al.) found a 7-fold increase in the risk of developing schizophrenia when exposed to influenza during the first trimester. No increased risk was found for exposure during the second and third trimester.
- Another study from 2008 (Structural brain alterations in schizophrenia following fetal exposure to the inflammatory cytokine interleukin-8 Ellman et al.) suggested that it was prenatal exposure to a type of protein - (proinflammatory cytokines, specifically interleukin-8) – produced by the body during viral infections, that can lead (in rare cases) to brain abnormalities.
- Last year, research by a team at UC Davis found that fever (from any cause) during pregnancy more than doubled the odds of having a child with autism or developmental delays (see Is Maternal Influenza or Fever During Pregnancy Associated with Autism or Developmental Delays? Results from the CHARGE (CHildhood Autism Risks from Genetics and Environment) Study Zerbo et al.)
- In November of last year, in Of Pregnancy, Flu & Autism, we saw a study that found a twofold increase in autism among children with prenatal influenza exposure, and a threefold increase in autism among children with prolonged prenatal fever exposure
It should be noted that these studies looked at relative risk increases, and that the absolute risk of offspring developing these psychiatric or developmental disorders later in life – regardless of exposure in the womb - is still fairly low.
Debated also is whether these disorders might be caused by an immune response to infection by the mother, or fetal exposure to the virus itself.
While the jury is still out, we’ve seen evidence that the influenza virus can be neurotropic - capable of infecting and damaging brain cells. For a recent review of this supposed link, see Revisiting The Influenza-Parkinson’s Link.
For these, and other reasons, the CDC and many other public health entities continue to stress the importance of seasonal flu vaccination for pregnant women.
In October of 2011, in IDSA: Flu Vaccines In Pregnancy, we saw several studies presented at the 49th Annual Meeting of the Infectious Diseases Society of America (IDSA) reaffirming the benefits and safety of maternal vaccination.
The CDC has synopsized these studies in:
Pregnancy and Influenza Vaccine Safety
Vaccines are drugs, and there is no such thing as a 100% safe and 100% effective drug. Even taking over-the-counter medicines entail some risks.
But the safety profile of flu vaccines is excellent, and serious side effects are exceedingly rare.
The overwhelming evidence shows that the real risk comes from the virus, not from the shot.