# 8357
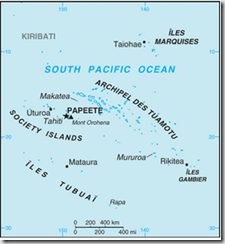
Ten days ago in Zika, Dengue & Unusual Rates Of Guillain Barre Syndrome In French Polynesia, we looked at the history of this (normally mild) emerging mosquito-borne virus, and at a recent outbreak in the South Pacific that – quite unusually – seemed to be linked to an increase in Guillain Barré Syndrome cases as well.
The CDC describes Guillain-Barré syndrome below:
What is Guillain-Barré syndrome (GBS)?
Guillain-Barré syndrome (GBS) is a rare disorder in which a person’s own immune system damages their nerve cells, causing muscle weakness and sometimes paralysis. GBS can cause symptoms that last for a few weeks. Most people recover fully from GBS, but some people have permanent nerve damage. In very rare cases, people have died of GBS, usually from difficulty breathing. In the United States, for example, an estimated 3,000 to 6,000 people develop GBS each year on average, whether or not they received a vaccination.
What causes GBS?
Many things can cause GBS; about two-thirds of people who develop GBS symptoms do so several days or weeks after they have been sick with diarrhea or a respiratory illness. Infection with the bacterium Campylobacter jejuni is one of the most common risk factors for GBS. People also can develop GBS after having the flu or other infections (such as cytomegalovirus and Epstein Barr virus). On very rare occasions, they may develop GBS in the days or weeks after getting a vaccination.
Who is at risk for developing GBS?
Anyone can develop GBS; however, it is more common among older adults. The incidence of GBS increases with age, and people older than 50 years are at greatest risk for developing GBS.
The ECDC’s summation of the Zika situation in French Polynesia (released March 3rd) follows:
Zika virus infection outbreak in The Pacific
In French Polynesia, 61 new suspected cases of Zika virus infection (ZIKAV) were recorded during the last week bringing the total number of suspected cases to 8 503. One additional case of Guillain-Barré syndrome has been reported. One case of ZIKAV in a returning traveller from Tahiti was confirmed by the Norwegian Institute of Public Health. The outbreak is declining in the majority of the islands.This is the second documented outbreak of ZIKAV in the Pacific. It is estimated that more than 29 000 cases sought medical care with Zika-like symptoms in French Polynesia since the beginning of the outbreak in October 2013.
Yesterday, the journal Eurosurveillance carried a Rapid Communications describing the first case of Guillain Barre (GBS) associated with ZIKAV infection in French Polynesia. While the exact link between ZIKAV (and/or Dengue) and GBS is undetermined, this region has reported a 20-fold increase in the neurological disorder during the recent epidemic.
E Oehler (
)1, L Watrin2, P Larre2, I Leparc-Goffart3, S Lastère4, F Valour1, L Baudouin5, H P Mallet6, D Musso7, F Ghawche2
Zika fever, considered as an emerging disease of arboviral origin, because of its expanding geographic area, is known as a benign infection usually presenting as an influenza-like illness with cutaneous rash. So far, Zika virus infection has never led to hospitalisation. We describe the first case of Guillain–Barré syndrome (GBS) occurring immediately after a Zika virus infection, during the current Zika and type 1 and 3 dengue fever co-epidemics in French Polynesia.
<SNIP Extensive Case Report>
Discussion and conclusion
During this ongoing Zika fever outbreak in French Polynesia, we report the first case of GBS developing seven days after an influenza-like illness evoking ZIKA infection. Based on IgM/IgG serological results and PNRT which, according to our experience, is reliable and specific enough to differentiate a recent ZIKA infection from cross-reactions due to former infections to DENV, we believe that this is the first case of hospitalisation because of a severe ZIKA infection.
Since the beginning of this epidemic, and as up to 8,200 cases of ZIKA infection have already been reported of a 268,000 total population, the incidence of GBS has been multiplied by 20 in French Polynesia (data not shown), raising the assumption of a potential implication of ZIKA.
Underlying physiopathological mechanisms of Zika-related GBS is unknown, and could be of immunological origin as described with other infectious agents [18]. There is also no explanation for the emergence of this previously undescribed complication, which could lie in a genetic evolution of the virus to a more pathogenic genotype, or a particular susceptibility in the Polynesian population.
As suggested by DENV and ZIKA serological tests in our patient, the simultaneous epidemics of type 1 and 3 dengue fever may also be a predisposing factor for developing GBS during Zika fever, as DENV infection had also been associated with GBS [19,20]. Our patient, like part of others who also presented a GBS, harboured serological markers of resolute dengue and recent ZIKA infections. This raises the hypothesis of a sequential arboviral immune stimulation responsible for such unusual clustering of GBS cases during concurrent circulation of ZIKA and two dengue serotypes. The risk of developing GBS would be consequently underlain by a specific sequence of DENV and ZIKA infections.
Therefore in endemic areas, clinician should be aware of the risk of diffuse demyelinating disorder in case of ZIKA infection.