#12,404
When the next influenza pandemic virus emerges and begins to spread around the world, the CDC, HHS, WHO and other partners will work to contain the outbreak at its source (if possible), to slow its spread internationally (again, if possible), and begin to work on a vaccine.
A vaccine - while viewed as the best response to a pandemic, will take time. How much time, will depend on a lot of factors.Despite improved vaccine manufacturing technologies, we would have to get very lucky to have any significant quantity of vaccine available for the general public in less than six months.
A novel virus may require 2 shots - a month apart - to invoke an adequate immune response, and that assumes an effective vaccine can be made at all.
- Despite more than a decade of trying, there is still no safe and effective SARS vaccine. The same goes for MERS, which emerged five years ago (see Obstacles To A MERS Vaccine).
- Early H5N1 and H7N9 vaccines were both notoriously difficult to make, and only produced meager immune responses (see JAMA: Immune Response Of H7N9 Vaccine With & Without Adjuvant).
Add in the inevitable global scramble for a limited supply of any vaccine, the logistics of deploying said vaccine to billions of people in a short period of time . . . and well - the TV and movie cliche where some valiant scientist creates, tests, and distributes a vaccine in the nick of time is a pretty optimistic scenario.
This isn't to dismiss the importance of a vaccine. Pandemics tend to come in waves. The 1918 pandemic - which killed between 50 and 100 million people - came in three distinct waves, over an 18 month period.
Even if a vaccine isn't available for the first wave, it could save millions of lives in the waves that follow.But until a vaccine is widely available, the goal is to slow the spread of a pandemic virus, to limit its impact, and to try to save as many lives as possible through the use of NPIs - Nonpharmaceutical Interventions.
The CDC’s Nonpharmaceutical Interventions (NPIs) webpage defines NPIs as:
Nonpharmaceutical interventions (NPIs) are actions, apart from getting vaccinated and taking medicine, that people and communities can take to help slow the spread of illnesses like influenza (flu). NPIs are also known as community mitigation strategies.
While some may scoff at their effectiveness, we have a real-world example during the worst flu pandemic in recorded history - the 1918 Spanish flu.
The chart above, taken from the PNAS journal article entitled Public Health Interventions and Pandemic Intensity During the 1918 Influenza Pandemic, illustrates what happened in two American cities during the 1918 pandemic.
- The sharp, but much shorter pandemic wave depicted by the solid line occurred in Philadelphia, where relatively few steps were taken by the public health department to slow the spread of the disease (they even ok'd a massive Liberty Loan parade on September 28th).
- The dotted line represents St. Louis, which closed schools early and where the Health Department prohibited public gatherings in places like theaters, churches, and restaurants.
At its worst, the percentage of excess of people afflicted in the city of Philadelphia was 5 times greater than what St. Louis experienced. The burden on hospitals, mortuaries, and practically all segments of the economy was certainly far greater.
None of this is a new concept, and we were discussing these issues 10 years ago when the previous Community Mitigation Guidelines were released.
This is why the primary goal of the HHS/CDC's 2017 revised Community Mitigation Guidelines to Prevent Pandemic Influenza - which we've already looked at twice yesterday (see here, and here) - is to slow the spread of any pandemic outbreak, in hopes of limiting its impact on hospitals, essential workers, infrastructure, and ultimately reducing the death toll.
An excerpt from the summary reads:
Purpose
The purpose of these guidelines is to help state, tribal, local, and territorial health departments with prepandemic planning and decision-making by providing updated recommendations on the use of NPIs.
These recommendations have incorporated lessons learned from the federal, state, and local responses to the influenza A (H1N1)pdm09 virus pandemic (hereafter referred to as the 2009 H1N1 pandemic) and findings from research. Communities, families and individuals, employers, and schools can create plans that use these interventions to help slow the spread of a pandemic and prevent disease and death.
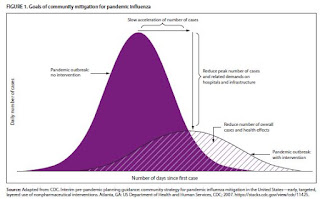
Specific goals for implementing NPIs early in a pandemic include slowing acceleration of the number of cases in a community, reducing the peak number of cases during the pandemic and related health care demands on hospitals and infrastructure, and decreasing overall cases and health effects ( Figure 1).
When a pandemic begins, public health authorities need to decide on an appropriate set of NPIs for implementation and to reiterate the importance of personal protective measures for everyday use (e.g., voluntary home isolation of ill persons [staying home when ill], respiratory etiquette, and hand hygiene) and environmental cleaning measures (e.g., routine cleaning of frequently touched surfaces), which are recommended at all times for prevention of respiratory illnesses ( Table 1).(Continue . . . .)
Personal protective measures reserved for pandemics (e.g., voluntary home quarantine of exposed household members [staying home when a household member is ill] and use of face masks by ill persons) also might be recommended (Table 1). A more difficult decision is how and when to implement community-level NPIs that might be warranted but are more disruptive (e.g., temporary school closures and dismissals, social distancing in workplaces and the community, and cancellation of mass gatherings) (Table 1).
These decisions are made by state and local officials on the basis of conditions in the applicable jurisdictions, with guidance from CDC (according to pandemic severity and potential efficacy) and governing authorities (1). Prepandemic planning, along with community engagement, is an essential component of these decisions ( Table 2).
Although there may be other pharmaceutical options - like antivirals - available at the start of a pandemic, those will be in finite supply and are not a panacea for infection. Prevention is always better than treatment, but never more so than during a pandemic, when treatment options may quickly become limited.
Hospital beds, ventilators, even hospital staff - may all be in short supply during a pandemic (nurses get sick, too) - which makes it all the more imperative we flatten the curve - even if it means extending the duration of a pandemic wave.
While telling people to wash their hands, cover their coughs, avoid crowds, and stay home while sick may seem like a weak response to a pandemic - in truth, they (and other more disruptive measures like school closures, cancellation of public events, etc.) may be our most powerful weapons in any pandemic.
But they must be properly applied, else they could do more harm than good.It's neither practical or desirable to simply shut everything down at the first sneeze, and try to wait out what could be a year (or longer) pandemic. Very few are equipped to do so, and besides, someone has to keep the lights on, deliver the food, refine the fuel, police the streets, take care of the sick and injured . . . and do the thousands of other things that hold civilization together.
We'll have to find ways to live and work as safely as possible during a pandemic. Else the virus could quickly become the least of our problems.
Which is the point of these new guidelines. A severe pandemic will require some difficult, and likely unpopular, decisions on the part of public health and government officials. If those decisions were easy, or clear cut, I suspect it wouldn't take near 160 pages to help explain the scientific rationale behind them.
It's not an exact science, and no one should expect that all will go smoothly during a pandemic, even with these new guidelines.But at least we have the experience of the 2009 pandemic under our belts, along with 10 years of additional science, to augment and improve the previous set of guidelines. For a look as some of the research on NPIs over the past few years, you may wish to revisit:
Study: Effectiveness of NPIs Against ILI's
Michigan NPI Study: A Closer Look
Study: Efficacy Of Hand Hygiene Alone Against Influenza Infection
NPI’s and Influenza
Study: NPI's Can Help Prevent Spread Of Flu-Like Illnesses