 |
| Credit CDC |
#13,031
While we spend a good deal of time talking about exotic infections (novel flu, Ebola, Zika, Dengue, C. auris, etc.) in this blog, seasonal influenza - which comes knocking every winter - looks like it is trying to kick in the door this year.
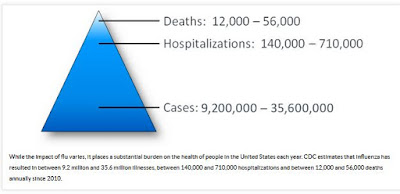
During a `bad’ flu year, the potential exists for seeing tens of thousands of flu deaths, and hundreds of thousands of flu hospitalizations across North America.Globally, it has been estimated that seasonal flu kills between 291,000 and 646,000 people each year (see The Lancet: Estimates Of Global Seasonal Flu Respiratory Mortality). For every flu death in the United States, however, there are likely 15-20 hospitalizations and another 600-800 mild to moderate cases.
 |
| https://www.cdc.gov/flu/about/disease/burden.htm |
Of these 12 to 36 million people affected, roughly 10% will live alone, a complicating factor we looked at last Friday in Yes, We Have No Pandemic . . . But Line Up A Flu Buddy Anyway.
But with - or without a support system, millions of people either already are - or will be - dealing with flu at home this winter.It is therefore important that everyone know how to deal with flu at home, what the warning signs are that a flu victim needs to go to the hospital, and what home meds work . . . and which ones can make matters worse.
Our first stop is the CDC's 21 page (PDF) Home Flu Treatment Guide, which covers everything from knowing the symptoms of flu, to setting up (and cleaning) a sick room, to when it is time to seek medical help.
 |
| PDF FILE |
(EXCERPT)
Know the emergency warning signs
There are “emergency warning signs” that should signal anyone to seek medical care urgently. Seek care if the sick person has ANY of the signs below.
In children, emergency warning signs that need urgent medical attention include:
• Fast breathing or trouble breathingIn addition to the signs above, get medical help right away for any infant who has any of these signs:
• Bluish skin color
• Not drinking enough fluids
• Not waking up or not interacting
• Being so irritable that the child does not want to
be held
• Flu-like symptoms improve but then return with
fever and worse cough
• Fever with a rash
• Being unable to eat
• Has trouble breathing
• Has no tears when crying
• Significantly fewer wet diapers than normal
In adults, emergency warning signs that need urgent medical attention include:
• Difficulty breathing or shortness of breath
• Pain or pressure in the chest or abdomen
• Sudden dizziness
• Confusion
• Severe or persistent vomiting
• Flu–like symptoms that improve but then return
with fever and worse cough
This is an excellent guide, and well worth downloading and printing out, or keeping as a reference PDF on your phone/tablet/computer.
It is important to remember that `cardiac symptoms' particularly in older flu victims, may appear in the days to weeks following a severe respiratory infection.Last year, in Int. Med. J.: Triggering Of Acute M.I. By Respiratory Infection we looked at research from the University of Sydney that found the risk of a heart attack is increased 17-fold in the week following a respiratory infection such as influenza or pneumonia (see ‘Tis The Cardiac Season).
If you happen to be a member of a `high risk group' and get the flu, it is important to contact your doctor immediately, as there are antiviral medications which can lessen the duration and severity of your symptoms (see CDC HAN: Seasonal A(H3N2) Flu Activity & Antiviral Treatment of Patients with Influenza).
High Risk groups include:
- children younger than 2 years (although all children younger than 5 years are considered at higher risk for complications from influenza, the highest risk is for those younger than 2 years)
- adults aged 65 years and older
- persons with chronic pulmonary (including asthma), cardiovascular (except hypertension alone), renal, hepatic, hematological (including sickle cell disease), and metabolic disorders (including diabetes mellitus), or neurologic and neurodevelopment conditions (including disorders of the brain, spinal cord, peripheral nerve, and muscle such as cerebral palsy, epilepsy [seizure disorders], stroke, intellectual disability [mental retardation], moderate to severe developmental delay, muscular dystrophy, or spinal cord injury)
- people with immunosuppression, including that caused by medications or by HIV infection
- women who are pregnant or postpartum (within 2 weeks after delivery)
- people aged younger than 19 years who are receiving long-term aspirin therapy
- American Indians/Alaska Natives
- people with extreme obesity (i.e., body-mass index is equal to or greater than 40)
- residents of nursing homes and other chronic-care facilities
Each winter I try to write about the potential danger of certain types of OTC cold and flu medications as well. While generally safe if taken as directed, OTC medications are real drugs, and should only be taken when the rewards of using them outweigh the risks.
In 2016's A Reminder To Know Your Dose, we looked at the accidental overdose potential for acetaminophen (aka `Tylenol ®, APAP). Although it is one of the most popular OTC medications in the world, there is a relatively narrow margin between the maximum therapeutic dose and a potentially toxic (and sometimes fatal) overdose.
While well tolerated when taken as directed, APAP in larger doses is a hepatotoxin; it overwhelms and destroys the liver. In fact, APAP poisoning is the biggest cause of acute liver failure in the United States.A study published in 2011 in the American Journal of Preventive Medicine (see Emergency Department Visits for Overdoses of Acetaminophen-Containing Products) found that - in the United States alone – there were an estimated 78,414 ER visits each year due to acetaminophen poisoning.
Although most of these were intentional overdoses (69.8%), more than 13,000 ER visits were described as due to `therapeutic misadventures’ . . . or accidental overdoses.You'll find acetaminophen in hundreds of different cold remedies, making it easy to accidentally double (or triple) dose yourself.
While many parents were brought up in a time when it was deemed perfectly acceptable to give toddlers OTC cold remedies (or in the 1950's when my Grand Dad's `Rock & Rye' recipe was the `universal cure'), today most of those meds have been relabeled only for those over the age of 4. :
- In Kids, Colds, And OTC Meds we looked at the continuing trend of parents – against the advice of the CDC – to use OTC medications to treat cold and flu symptoms in toddlers under the age of four.
- We looked at inconsistent and confusing dosing instructions provided by many manufacturers of OTC medications in JAMA: Inconsistent Dosing Instructions For OTC Meds.
- And in Inappropriate Use Of OTC Medicines In Children we looked at a report that inappropriate use, and incorrect dosing of OTC meds lead to a large number of accidental drug poisonings each year.
Of course, the time to download the CDC's guide, pick up sick room supplies, and purchase any OTC meds you may need is now - not after you're already sick (and contagious) with the flu.
If you are sick, stay home. Flu doesn't need any extra help spreading the misery.
