#13,135
Today's FluView report is out, and once again the news is pretty bad. In fact, this year's flu season is on track to equal or exceed the worst non-pandemic flu seasons of the past 15 years.
While there were hopes that the flu season was about to peak, this week's numbers (which reflect flu activity 1 to 2 weeks ago) show that influenza continues to increase across much of the country, although influenza H3N2 is beginning to decline in some regions while Influenza B is starting to climb.
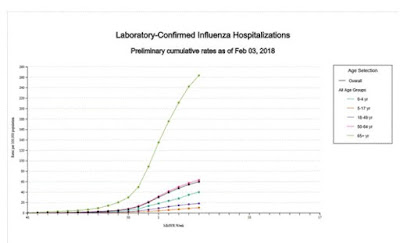
Even so, the cumulative number of hospitalizations this winter is rapidly approaching the number posted at the end of the 2014-15 high severe season, and there could be another 6 to 10 weeks of flu remaining.
Remarkably, ILI consultation rates (7.7%) now equal what was seen at the height of the H1N1 pandemic in 2009.
The only `good' news is that the number of H3N2 cases continues to drop (only 70%) while Influenza B and H1N1 slowly rise. Although these strains can also produce severe illness, the effectiveness of this year's vaccine against those strains is expected to be much higher.
The `bad' news is, that even if you've had the H3N2 flu already this winter, it is possible to be infected again by either H1N1 or Influenza B.Some highlights from today's report follow:
2017-2018 Influenza Season Week 5 ending February 3, 2018
All data are preliminary and may change as more reports are received.Synopsis:
During week 5 (January 28-February 3, 2018), influenza activity increased in the United States.
- Viral Surveillance: The most frequently identified influenza virus subtype reported by public health laboratories during week 5 was influenza A(H3). The percentage of respiratory specimens testing positive for influenza in clinical laboratories remained elevated.
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was above the system-specific epidemic threshold in the National Center for Health Statistics (NCHS) Mortality Surveillance System.
- Influenza-associated Pediatric Deaths: Ten influenza-associated pediatric deaths were reported.
- Influenza-associated Hospitalizations: A cumulative rate of 59.9 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported.
- Outpatient Illness Surveillance:The proportion of outpatient visits for influenza-like illness (ILI) was 7.7%, which is above the national baseline of 2.2%. All 10 regions reported ILI at or above region-specific baseline levels. New York City, the District of Columbia, Puerto Rico and 43 states experienced high ILI activity; three states experienced moderate ILI activity; two states experienced low ILI activity; and two states experienced minimal ILI activity.
- Geographic Spread of Influenza:The geographic spread of influenza in Puerto Rico and 48 states was reported as widespread; two states reported regional activity; the District of Columbia and Guam reported local activity; and the U.S. Virgin Islands reported sporadic activity.
Another 10 pediatric deaths were reported in the last week, bringing this season's total to 63. Pediatric deaths - while reportable - likely underestimate the true number, and are often delayed by several weeks in being reported to the CDC.
P&I Mortality is another lagging indicator. Not only are these numbers from 3 weeks ago, instead of last week like the rest of this report, many hospitalized patients may survive for weeks before succumbing to their illness.
This graph is likely to climb higher, but for now 10.1% of deaths last week in the United States were attributed to influenza and/or pneumonia.
As always, it isn't too late to get the flu shot. And with influenza B and H1N1 rising, it could still offer some valuable protection. But most of all, now is the time to practice good flu hygiene.
Stay home if you are sick, avoid crowds, wash your hands frequently, and cover your coughs and sneezes.The same virus that only made you mildly ill could prove deadly to someone else. Don't help it break any more records. And with a month or more of flu ahead, remember: