Laboratory-confirmed cyclosporiasis cases by week of onset — United States, June 1–September 10, 2013 – CDC MMWR
# 7928
While fairly common in developing tropical, or sub-tropical countries, Cyclosporiasis – an infection usually acquired through consuming food or water contaminated with Cyclospora cayetanensis - is relatively rare in the United States.
Unlike the more common cryptosporidium, which can be easily be passed from human-to-human, Cyclospora is rarely transmitted directly from an infected host. Hosts infected with Cyclospora shed unsporulated (non-infective) cysts in their stool which require days or even weeks to mature into infectious agents.
Over the summer, we witnessed a multi-state outbreak of Cyclosporiasis, which I blogged about several times (see here, here, and here). Infection with this parasite is characterized by prolonged bouts of watery diarrhea, which may persist or reoccur over a period of weeks. According to the CDC, Trimethoprim/sulfamethoxazole (TMP/SMX), is the recommended treatment, although they state:
Most people who have healthy immune systems will recover without treatment. If not treated, the illness may last for a few days to a month or longer. Symptoms may seem to go away and then return one or more times (relapse).
Anti-diarrheal medicine may help reduce diarrhea, but a health care provider should be consulted before such medicine is taken. People who are in poor health or who have weakened immune systems may be at higher risk for severe or prolonged illness.
This outbreak slowed, and finally ended, by the end of August. Yesterday, the CDC’s MMWR carried a brief post-mortem on the outbreak, which identified not one – but at least two separate outbreaks – and that `the food item associated with illness in Texas was different from that implicated in restaurant-associated cases in Iowa and Nebraska’.
Notes from the Field: Outbreaks of Cyclosporiasis — United States, June–August 2013
Weekly
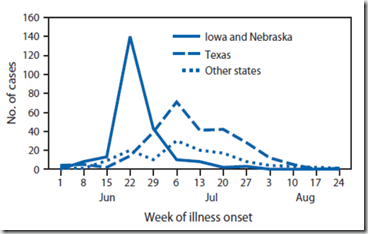
November 1, 2013 / 62(43);862-862During June–August 2013, CDC, state and local public health officials, and the Food and Drug Administration (FDA) investigated an unusually large number of reports of cyclosporiasis (compared with annual reports to the National Notifiable Disease Surveillance System [e.g., 123 cases in 2012]), an intestinal infection caused by the parasite Cyclospora cayetanensis (1). By September 20, CDC had been notified of 643 cases from 25 states, primarily Texas (278 cases), Iowa (153), and Nebraska (86). Investigations in Iowa and Nebraska showed that restaurant-associated cases in these two states were linked to a salad mix that contained iceberg lettuce, romaine lettuce, red cabbage, and carrots (2). Most patients in Iowa and Nebraska became ill during June 15–29; cases reported during July and August were primarily from Texas (Figure).
CDC collaborated with state and local public health officials in Texas and the FDA to investigate a cluster of illnesses among patrons of a Mexican-style restaurant in Fort Bend County, Texas (restaurant A). A case of restaurant A–associated gastroenteritis was defined as gastrointestinal illness in a person who had eaten at restaurant A after June 1, 2013. Of 30 persons who ate at restaurant A, 22 had laboratory-confirmed C. cayetanensis infections, and eight had no laboratory confirmation. To identify the source or sources of the infections, a case-control study using 21 case-patients (15 laboratory-confirmed and six probable) with known meal dates and 65 controls matched by restaurant A meal date was conducted.
Case-patients and controls were asked about the meals they ate at restaurant A, using the menu. Ingredient-level analyses were conducted using meal consumption data and restaurant A recipes to identify four fresh produce ingredients with a statistically significant association with illness: fresh cilantro (matched odds ratio [mOR] = 19.8; 95% confidence interval [CI] = 4.0–>999), whole onions (mOR = 15.3; CI = 2.1–697.7), garlic (mOR = 10.7; CI = 1.5–475.4), and tomatoes (mOR = 5.5; CI = 1.1–54.1). Only fresh cilantro was consumed by all case-patients included in the study. In addition, of the four restaurant-produced salsas served at restaurant A, three containing fresh, uncooked cilantro were associated with illness: hot salsa (mOR 8.0; CI = 2.3–31.4), side salsa (mOR 5.7; CI = 1.6–23.7), and fire salsa (mOR 3.5, CI = 1.1–12.7). Case-patients also more commonly than controls reported eating salsa ranchera, which contained fresh cooked cilantro, but the association was not statistically significant: (mOR = 6.0; CI = 0.7–75.2).
Traceback information indicated that Puebla, Mexico, was a source of fresh cilantro served to ill persons at restaurant A. Lettuce served at restaurant A was neither sourced from the same producer implicated in the outbreak investigation in Iowa and Nebraska nor was it associated with illness. Additionally, restaurant A did not use red cabbage or carrots. Taken together, data from tracebacks and epidemiologic investigations in Texas, Iowa, and Nebraska indicate that more than one outbreak of cyclosporiasis occurred during summer 2013 in the United States, and that the food item associated with illness in Texas was different from that implicated in restaurant-associated cases in Iowa and Nebraska.