#13,025
Although Saudi Arabia only reported 8 MERS-CoV cases in December, the virus remains a threat to public health on the Arabian peninsula, and the exported case reported over the weekend (see Malaysia: MOH Announces Imported MERS-CoV Case) is a reminder that MERS can threaten other parts of the world as well.
The actual number of MERS cases that go unidentified in Saudi Arabia and surrounding countries is a matter of much debate, but a handful of studies suggest that number may be sizable.
- In November of 2013, we looked at a study published in The Lancet Infectious Diseases, that estimated for every case identified, there are likely 5 to 10 that go undetected.
- In 2015 when Saudi Arabia had recorded fewer than 1200 MERS cases, a seroprevalence study(see Presence of Middle East respiratory syndrome coronavirus antibodies in Saudi Arabia: a nationwide, cross-sectional, serological study by Drosten & Memish et al.,) suggested nearly 45,000 might have been infected.
- And in 2016, in EID Journal: Estimation of Severe MERS Cases in the Middle East, 2012–2016, we saw a study that suggested the number of severe cases is 2.3-times higher than the total number of all laboratory-confirmed cases combined (including mild and asymptomatic) cases in the region.
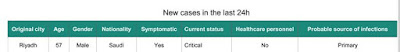
Today we have another of those community acquired `primary' cases with no known risk exposure, this time in a 57 y.o. male who is listed in critical condition in Riyadh.
Although MERS has not (yet) become efficiently transmissible enough (at least in a community setting) to spark a genuine epidemic, a recent study (see A Pandemic Risk Assessment Of MERS-CoV In Saudi Arabia) - which appears in the November issue of the Saudi Journal Of Biological Sciences - provides a detailed statistical analysis of MERS-COV cases reported in Saudi Arabia from May 2013 to May 2015.
While this study reported a sub-critical R0 (R: 0.85–0.97) across all regions, during the study period the central and western regions flirted with epidemic level R0 (R: 1.08–1.12) numbers.The R or R0 (pronounced R-naught) is the basic reproduction number; the epidemiological yardstick by which transmission of an infectious disease is measured. Essentially, the number of new cases in a susceptible population likely to arise from a single infection.
With an R0 below 1.0, a virus (as an outbreak) begins to sputter and dies out.All of which means, while apparently still not ready for prime time, MERS-CoV wouldn't need to gain a whole lot more transmissibility to become a genuine pandemic threat.
Above 1.0, and an outbreak can have `legs’.
So we watch cases like today's, looking for any signs that the virus become more of a threat.