The chart above (Aug 2012) illustrates the sharp rise in pediatric deaths from flu-related complications during the 2009-2010 H1N1 pandemic seasons in the United States.
# 7571
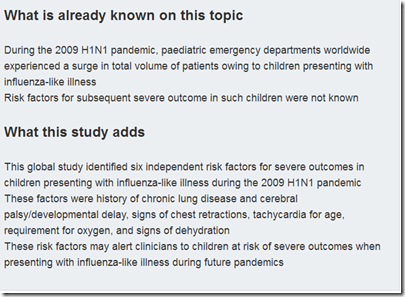
The BMJ has published this week research from an international team of medical scientists who looked at presenting symptoms and comorbidities of 265 pediatric cases from 79 emergency rooms in 12 countries presenting with the H1N1 pandemic flu.
The team was able to identify several factors that they could associate with a higher risk of severe infection, complications, or death.
It is hoped that these findings could help guide physician decisions on treatment of children, or their admission to the hospital, in future influenza outbreaks.
First a link to the study (which is available, in full, online) then some excerpts from a news release from the University of Auckland.
Research
Predictors of severe H1N1 infection in children presenting within Pediatric Emergency Research Networks (PERN): retrospective case-control study
BMJ 2013; 347 doi: http://dx.doi.org/10.1136/bmj.f4836 (Published 12 August 2013)
Cite this as: BMJ 2013;347:f4836
Stuart R Dalziel, paediatrician, John MD Thompson, senior research fellow, Charles G Macias, associate professor, Ricardo M Fernandes, paediatrician4, David W Johnson, professor, Yehezkel Waisman, professor, Nicholas Cheng, paediatrician, Jason Acworth, paediatrician, James M Chamberlain, professor, Martin H Osmond, professor, Amy Plint, associate professor, Paolo Valerio, paediatrician, Karen JL Black, paediatrician, Eleanor Fitzpatrick, research coordinator, Amanda S Newton, assistant professor, Nathan Kuppermann, professor, Terry P Klassen, professor for the Pediatric Emergency Research Networks (PERN) H1N1 working groupAbstract
(EXCERPT)
Main outcome measures Severe outcomes included death or admission to intensive care for assisted ventilation, inotropic support, or both. Multivariable conditional logistic regression was used to compare cases and controls, with effect sizes measured as adjusted odds ratios.
Results 151 (57%) of the 265 cases were male, the median age was 6 (interquartile range 2.3-10.0) years, and 27 (10%) died. Six factors were associated with severe outcomes in children presenting with influenza-like illness: history of chronic lung disease (odds ratio 10.3, 95% confidence interval 1.5 to 69.8), history of cerebral palsy/developmental delay (10.2, 2.0 to 51.4), signs of chest retractions (9.6, 3.2 to 29.0), signs of dehydration (8.8, 1.6 to 49.3), requirement for oxygen (5.8, 2.0 to 16.2), and tachycardia relative to age).
Conclusion These independent risk factors may alert clinicians to children at risk of severe outcomes when presenting with influenza-like illness during future pandemics.
The news release from the University of Auckland provides some additional background on this study.
Top risk factors identified for children during influenza pandemics
14 August 2013
Auckland medical scientists have helped to identify crucial risk factors for children most susceptible to life threatening infections from the H1N1 influenza virus.
Lead study author Dr Stuart Dalziel and senior research fellow Dr John Thompson from The University of Auckland worked with an international team of paediatric specialists to identify the risk factors.
It is the first study to detail which clinical factors in children at hospital arrival with influenza-like illness and H1N1 infection, are associated with the progressive risk to either severe infection or death.
<SNIP>
The study, which assessed each patient’s clinical history and physical examination, identified the following predictors of severe H1N1 infection and potentially fatal outcomes in children:
- History of chronic lung disease
- History of cerebral palsy/developmental delay
- Signs of chest retractions (difficulty breathing)
- Signs of dehydration
- Requires oxygen to keep blood levels normal
- Heart rate that exceeds normal range (tachycardia) relative to age
“Having a more accurate idea of what to look for in paediatric cases, especially during a pandemic, would be especially important to clinicians because it provides crucial guidance for those who would be trying to direct the appropriate levels of treatment for many patients in a short time,” said one of the study’s co-authors Nathan Kuppermann, professor and chair of emergency medicine at the University of California.
We’ve seen earlier studies on the impact of the 2009 H1N1 pandemic on children, some of which have produced similar findings.
Study: Kids, Underlying Conditions, And The 2009 Pandemic Flu
Lancet: Pediatric Mortality Related To Pandemic H1N1
Study: Pediatric Neurological Complications With H1N1
While it is axiomatic that - `if you’ve seen one flu pandemic . . . you’ve seen one flu pandemic’ - many of the lessons learned from the last pandemic are still likely to prove useful during the next global health crisis.
Even if the next pandemic differs substantially from what we went through in 2009.