# 9339
One of the `moving targets’ in the global public health response to Ebola has been what constitutes a `low risk exposure’ vs. a `high risk exposure’, and what kind of monitoring, or movement restrictions, are appropriate.
Previously, we’ve looked at the CDC’s original guidance (see CDC Issues New Ebola Case Definitions) along with some of updates (see CDC Updated Interim Guidance On Ebola) over time. In response to the Dallas travel confusion involving HCWs who had treated the index case, the State of Ohio issued their own, stricter rules (see Ohio Daily Ebola Contact Report – Oct 19th).
Today the ECDC has issued it’s own set of definitions of low vs high risk exposures, and their recommendations on the monitoring of contacts. They do state, however, that Implementation may be modified in accordance with the public health assessment carried out by the public health officer interviewing the contacts.
Click the link below to download the full PDF File.
Public health management of persons having had contact with Ebola virus disease cases in the EU
22 October 2014(EXCERPTS)
Definition of contact persons
A contact person of an EVD case is a person not currently presenting symptoms, who has or may have been in contact with an EVD case, with bodily fluids of a case, or with a soiled environment. The associated risk of infection depends on the level of exposure, which will in turn determine the type of monitoring.
1. Contact persons with low-risk exposure; examples:
• Casual or physical contact with a feverish but ambulant and self-caring EVD case (e.g. sharing a seating area or public transportation, including airplane transport; receptionist tasks; etc.)
• Close, face-to-face or physical contact with a case who is not coughing or vomiting.
• Household, classroom or office contact.
2. Contact persons with high-risk exposure; definition2:• Close face-to-face contact (e.g. within one metre) without appropriate personal protective equipment (including eye protection) with a probable or confirmed case who is coughing, vomiting, bleeding, or has diarrhoea.
• Direct contact with bodily fluids or any materials soiled by bodily fluids from a probable or confirmed case.
• Percutaneous injury (e.g. with a needle) or mucosal exposure to bodily fluids, tissues or laboratory specimens of a probable or confirmed case.
• Participation in funeral rites having direct contact with human remains (including bodily fluids) of a case in or from an area with community transmission without appropriate personal protective equipment.
• Having had unprotected sexual contact with a case within three months of the case recovering from EVD.
• [Having had direct contact with bushmeat, bats or primates, living or dead, from affected areas.] – no relevance to contact management.3. Healthcare workers with occupational exposure
• Occupational exposure of a healthcare worker, including laboratory workers, involved in caring for a confirmed EVD patient using appropriate personal protective equipment. Contact with EVD patients using appropriate personal protective equipment is considered to be low-risk exposure. However, given the continuous nature of the occupational exposure involved in caring for patients, such exposures should be dealt with as high-risk exposures.Monitoring of contacts
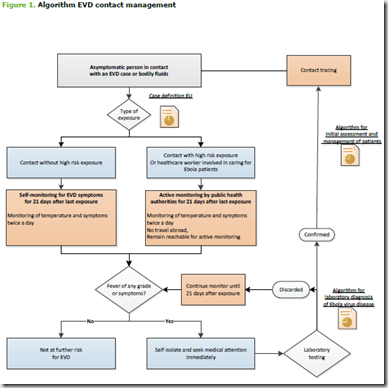
Figure 1 describes the monitoring of contacts and the actions to take in the event of a contact developing symptoms.
Public health authorities can, depending on the specific situation, support, promote or implement further restrictions (e.g. voluntary limitation of contacts by the person, or avoiding contact with crowds).
The contact tracing and management are based on the following current knowledge:• The incubation period of Ebola viruses can be as long as 21 days.
• Only symptomatic patients can transmit the infection. Infectiousness starts from the onset of symptoms.
• Transmission may occur through direct contact with the patient or blood and other bodily fluids of the patient.
• Dead bodies and their blood and bodily fluids remain infectious.
• There is no evidence of airborne transmission, but precautions are warranted when aerosol-generating symptoms (such as vomiting) are present or aerosol-producing procedures are performed.
• Transmission via inanimate objects contaminated with infected bodily fluids (fomites) is possible.
Main actions for contact persons• Contact with low-risk exposure:
− Self-monitoring for EVD symptoms, including fever of any grade, for 21 days after last exposure. Public health authorities may do more, depending on the specific situation.• Contact with high-risk exposure:
− Active monitoring for EVD symptoms, including fever of any grade, for 21 days after last exposure by public health authorities;
− No travel abroad;
− Remaining reachable for active monitoring;
− Restriction of contacts (voluntary self-quarantine or imposed) to be considered in the event of very high-risk exposure.• Healthcare worker with occupational exposure:
− Occupational health surveillance of healthcare workers should be enhanced.Contact persons should immediately self-isolate and contact health services in the event of any symptom appearing within 21 days. If no symptoms appear within 21 days of last exposure the contact person is no longer considered to be at risk of developing EVD.
Contact management steps after a case is identified
The steps are contact listing (and classification of the contact as having had low- or high-risk, or occupational exposure), contact tracing, contact assessment and management, and follow-up by an outbreak control team