Credit Wikipedia
# 10,556
The Journal Nature has published a new study, and the NIH has published an overview, on research that has found a fascinating (and unexpected) role of the soft palate in the adaptation, evolution and transmission of influenza viruses.
Since we’ve discussed receptor binding often in the past (see here, here, here, here and here for just a few), and the NIH announcement does a good job of describing both the background and this research, I’ll simply provide a link to the study (much of which is behind a pay wall), and then a link and some excerpts from the detailed NIH press release.
First a link to the Abstract in Nature.
The soft palate is an important site of adaptation for transmissible influenza viruses
Seema S. Lakdawala, Akila Jayaraman, Rebecca A. Halpin, Elaine W. Lamirande, Angela R. Shih, Timothy B. Stockwell, Xudong Lin, Ari Simenauer, Christopher T. Hanson, Leatrice Vogel, Myeisha Paskel, Mahnaz Minai, Ian Moore, Marlene Orandle, Suman R. Das, David E. Wentworth, Ram Sasisekharan & Kanta Subbarao Affiliations
Nature (2015) doi:10.1038/nature15379
Published online 23 September 2015
This from the NIH. Follow the link to read the whole fascinating story.
Embargoed for Release: Wednesday, September 23, 2015, 1 p.m. EDT
NIH researchers find role for soft palate in adaptation of transmissible influenza viruses
National Institutes of Health scientists and their colleagues identified a previously unappreciated role for the soft palate during research to better understand how influenza (flu) viruses acquire the ability to move efficiently between people. In studies using ferrets, the team collected evidence that this patch of mucous-coated soft tissue separating the mouth from the nasal cavity is a key site for the emergence of flu viruses with a heightened ability to spread through the air. The finding could aid efforts to define the properties governing flu virus transmissibility and predict which viruses are most likely to spark pandemics.
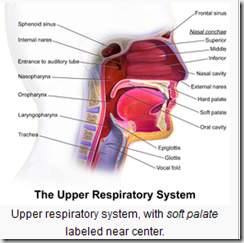
Flu viruses enter cells by binding to sialic acids on surface glycoproteins. In ferrets, pigs, and people, the nasopharyngeal surface of the soft palate contains regions of densely packed long-chain a2,6 sialic acid molecules (shown in green) where influenza viruses with airborne transmissibility can outcompete less transmissible virus. Credit: NIAID
The research was led by Kanta Subbarao, M.D., of NIH’s National Institute of Allergy and Infectious Diseases (NIAID), and Ram Sasisekharan, Ph.D., of Massachusetts Institute of Technology, Cambridge. Their report is published online in the journal Nature.
Flu infection in mammals starts when an influenza virus protein called hemagglutinin binds to sialic acid (SA) molecules on the tops of chain-like proteins that thickly line tissue throughout the respiratory tract. Flu viruses adapted to humans and other mammals bind preferentially to a type of SA called alpha 2,6 SA (α2,6 SA), which is the predominant form found in the upper respiratory tract of mammals, while avian flu viruses bind best to a form, α2,3 SA, that predominates in birds.
Dr. Subbarao and her colleagues began their research by making four mutations in the hemagglutinin of the flu strain responsible for the 2009 influenza pandemic, a strain notoriously good at spreading from person to person. The intent of introducing the mutations was to make the virus preferentially bind to bird-type SA and, presumably, be less transmissible via air than the original virus. They then used the engineered virus to infect a group of ferrets, which are widely used as a model of human influenza infection. The next day, uninfected ferrets were placed in cages separated from infected ferrets by a perforated barrier. Nasal secretions were collected from all of the animals for two weeks.
“To our surprise,” said Dr. Subbarao, “the engineered flu virus was transmitted by the airborne route to uninfected ferrets just as well as the original non-mutated virus.”
To understand this unexpected result, the researchers sequenced viral genetic material obtained from the ferret nasal washes. The sequencing was done by a team at the J. Craig Venter Institute, Rockville, Maryland. They discovered that airborne transmission was associated with a single genetic change in the engineered virus’s hemagglutinin that gave it the ability to bind to mammalian-type α2,6 SA of a particular class (long chain) without the loss of the other introduced changes that had made it a α2,3 SA binding type. This genetic reversion, Dr. Subbarao noted, appears to have occurred within 24 hours of administering the engineered flu virus to the experimentally infected ferrets. Subsequently, they passed it on to uninfected ferrets in the adjacent cages.
Next, the team looked at tissues from several locations in the ferrets’ upper and lower respiratory tract to more precisely define the location of the reverted, long chain α2,6 SA-binding virus. They infected groups of ferrets with the engineered virus — containing the same four mutations in hemagglutinin as in the first set of experiments — and three, five or seven days later, took tissue samples from various locations, including the soft palate.