#12,336
We are just one week shy of the 4th anniversary of the identification of a new avian influenza virus - H7N9 - in China. You can revisit that initial revelation in my March 31st, 2013 blog China: Two Deaths From H7N9 Avian Flu.
This first epidemic wave - which would grow to over 130 cases by May of 2013 - was the first real contender to the H5N1 virus, which had been the primary pandemic virus concern for over a decade.
This was more than a little surprising because HPAI H7 viruses - while known to be lethal to poultry - rarely caused more than mild illness in humans (see A Brief History Of H7 Avian Flu Infections).
And since China's H7N9 was an LPAI (Low pathogenic Avian Influenza) virus - basically benign in birds - it was considered even less likely to produce significant morbidity or mortality in humans.
Only it did. Among those sick enough to be hospitalized, nearly all were in serious or critical condition, and 30% succumbed.
For the past 4 years we've followed the evolution, and origins, of this avian threat. We've seen it eclipse H5N1's case counts - despite H5N1's 10 year head start - putting it atop the CDC's list of novel viruses with pandemic potential (see IRAT: Revisited).
Along the way we've seen evidence of its continual evolution - including signs of mammalian adaptations (see Eurosurveillance: Genetic Tuning Of Avian H7N9 During Interspecies Transmission) - and more recently its divergence into two genetically distinct lineages, and the emergence of an HPAI version of the virus (MMWR:Increase in Human Infections with Avian Influenza A(H7N9) In China's 5th Wave).
Yesterday Hong Kong media was filled with reports of recent discoveries by Hong Kong University - published in Nature Communications - that unlock some of the secrets behind H7N9's unlikely success as a human/avian pathogen.
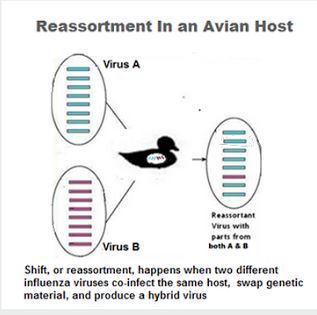
The culprit in this case appears to be a mutated nucleotide inherited from LPAI H9N2 during an early reassortment. This same mutation shows up in H5N6 and H10N8, also reassortant recipients of gene segments from H9N2, which both emerged in late 2013 and early 2014.
As we've discussed so many times over the years, whenever something `bad’ happens with an avian flu strain – if we look deep enough – we usually find highly promiscuous H9N2's genetic fingerprints at the scene.
In early 2014 The Lancet carried an on-point report entitled Poultry carrying H9N2 act as incubators for novel human avian influenza viruses..
Since 2013, reassortment with LPAI H9N2 viruses have `enabled' at least three new subtypes of avian flu (H7N9, H5N6, and H10N8) to emerge as human health threats. And there is no good reason to suppose that H9N2 couldn't help to spawn additional subtypes in the future.
Two reports on this - admittedly technical - open access study, published yesterday. First the link and abstract to the actual study, followed by a link and some excerpts from a University of Hong Kong press release.
An NS-segment exonic splicing enhancer regulates influenza A virus replication in mammalian cells
Xiaofeng Huang, Min Zheng, Pui Wang, Bobo Wing-Yee Mok, Siwen Liu, Siu-Ying Lau, Pin Chen, Yen-Chin Liu, Honglian Liu, Yixin Chen, Wenjun Song, Kwok-Yung Yuen & Honglin Chen(Continue . . .)
Abstract
Influenza virus utilizes host splicing machinery to process viral mRNAs expressed from both M and NS segments. Through genetic analysis and functional characterization, we here show that the NS segment of H7N9 virus contains a unique G540A substitution, located within a previously undefined exonic splicing enhancer (ESE) motif present in the NEP mRNA of influenza A viruses. G540A supports virus replication in mammalian cells while retaining replication ability in avian cells. Host splicing regulator, SF2, interacts with this ESE to regulate splicing of NEP/NS1 mRNA and G540A substitution affects SF2–ESE interaction. The NS1 protein directly interacts with SF2 in the nucleus and modulates splicing of NS mRNAs during virus replication. We demonstrate that splicing of NEP/NS1 mRNA is regulated through a cis NEP-ESE motif and suggest a unique NEP-ESE may contribute to provide H7N9 virus with the ability to both circulate efficiently in avian hosts and replicate in mammalian cells.
Many will find parts of this report tough sledding (I know I did), but luckily we've a pretty clear explanation of the their findings in the following report from HK University.
(EXCERPT)
22 Mar 2017
Research findings
The latest study published by the research team from State Key Laboratory for Emerging Infectious Diseases and Department of Microbiology, Li Ka Shing Faculty of Medicine, HKU, reveals the reason why H7N9 avian influenza virus possesses distinct fitness in circulating in avian host and causing human infections. The team performs analysis of the H7N9 virus genome collected from 2013 onwards and reveals that efficient infection of both avian and human cells by H7N9 viruses is supported by a unique nucleotide substitution (NS-G540A) in NS segment, where the mutation is located within a previously undefined exonic splicing enhancer (ESE). The researchers show that the position of this nucleotide is part of an RNA sequence motif that binds the human host cellular mechanism which supports virus replication and it is a common function in all influenza viruses. Host splicing regulator, SF2, regulates the virus replication efficiency as it interacts with ESE. Mutation in ESE identified in the viral genome of H7N9 virus enhances the ability of virus replication in mammalian cells.
The team proves that this mutation in viral genome provides H7N9 virus with the ability to both circulate efficiently in avian hosts and replicate in mammalian cells.
It is notable that human infections with H10N8 and H5N6 subtype avian influenza viruses contain the same mutation in the viral genome. This mutated nucleotide emerged in early 2000 in H9N2 strains and has since spread in avian influenza viruses, becoming the dominant genotype among avian influenza viruses from 2012 onwards. The H7N9 virus inherits the mutation from H9N2 virus. The 2013 H7N9 virus acquires internal genes from H9N2 virus and reassorts with haemagglutinin (HA) and neuraminidase (NA) genes from viruses present in wild birds, becoming the H7N9 virus that currently causes human infection.(SNIP)
Significance of the study
“This study provides a plausible mechanism to explain the molecular properties which allows H7N9 virus to infect humans while retaining the ability to circulate in avian species. It provides an important biomarker for monitoring the emergence and transmission of avian influenza viruses in humans and preventing human-to-human infection of the viruses. The mutation can also serve as a novel target of anti-influenza drug development,” says Professor Chen Honglin, Professor of State Key Laboratory for Emerging Infectious Diseases and Department of Microbiology, Li Ka Shing Faculty of Medicine, HKU.
(Continue . . . )
For more on H9N2's role in the evolution of other, more formidable avian flu viruses, you may wish to revisit:
- In 2014, in PNAS: Evolution Of H9N2 And It’s Effect On The Genesis Of H7N9 we looked at research that showed a new, better adapted genotype (G57) of the H9N2 virus had emerged in China – one that evades the poultry vaccines currently in use – and that it has become widespread among vaccinated Chinese poultry since 2010.
- In 2015, in EID Journal: Replication Of Avian H9N2 In Pet Birds, Chickens, and Mammals, Bangladesh, we looked at research that found the Bangladeshi version is a novel reassortant that has acquired some mammalian adaptations along the way, finding the virus replicates well in human and swine tissues.
- And almost a year ago we looked at A Canine H3N2 Virus With PA Gene From Avian H9N2 - Korea