#13,112
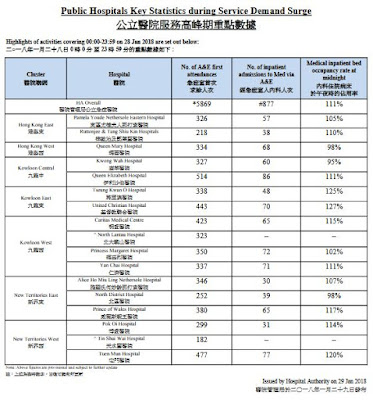
While North America is currently dealing with a mostly influenza A/H3N2 flu season, in Asia and in parts of Europe, Influenza B is leading the charge, and as we've seen (see Hong Kong Hospitals Inundated By Flu Cases), causing a good deal of morbidity and mortality.
Until a few years ago, Influenza B was viewed generally as a `less serious' infection than influenza A - affecting mainly children - and producing relatively mild illness in adults.An example of that belief comes from this 2009 study from Viral Immunology, called Influenza B virus causes milder pathogenesis and weaker inflammatory responses in ferrets than influenza A virus which opens with the statement:
Since then, however, we've seen a growing number of studies that challenge these old ideas, and show the severity of Influenza B infections to being comparable with Influenza A.It is unknown why the influenza B virus causes less severe clinical signs than the influenza A virus in humans. Here we show that influenza B virus induces a lower levels of inflammatory cytokines in the lungs of infected ferrets, and causes less pathological damage to their lung tissues than does influenza A virus.
In 2012, Lisa Schnirring of CIDRAP News wrote following story on a JID study called Myocardial Injury and Bacterial Pneumonia Contribute to the Pathogenesis of Fatal Influenza B Virus Infection.
Study finds influenza B may be more severe than thought
Lisa Schnirring |
Feb 01, 2012
Feb 1, 2012 (CIDRAP News) – An autopsy study involving influenza B infections revealed how histologically similar the disease is to fatal influenza A and how quickly it can kill, challenging the notion that it is milder than influenza A.(Continue . . . .)
The investigators, from the US Centers for Disease Control and Prevention (CDC), also found a high level of cardiac injury with fatal influenza B infections, especially in younger patients.
The research group said that comprehensive studies of influenza B deaths involving large series of patients and comparing those with and without bacterial pneumonia are lacking. Their findings appeared yesterday in the Journal of Infectious Diseases.
Two years later another important study was published, this time in the Clinical Infectious Diseases Journal, that once again challenged the old ideas about influenza B.
Comparing Clinical Characteristics Between Hospitalized Adults With Laboratory-Confirmed Influenza A and B Virus Infection
Su Su Sandra S. Chaves Alejandro Perez Tiffany D'Mello Pam D. Kirley Kimberly Yousey-Hindes Monica M. Farley Meghan Harris Ruta Sharangpani Ruth Lynfield ...
Clinical Infectious Diseases, Volume 59, Issue 2, 15 July 2014, Pages 252–255,
https://doi.org/10.1093/cid/ciu269 Published: 18 April 2014
ABSTRACT
We challenge the notion that influenza B is milder than influenza A by finding similar clinical characteristics between hospitalized adult influenza-cases. Among patients treated with oseltamivir, length of stay and mortality did not differ by type of virus infection.
The CDC, which partnered in this study, published the following summary:
New CDC Study Compares Severity of Illness Caused by Flu A and B Viruses
Influenza B virus infections can be just as severe as influenza A virus infections
As late-season influenza B viruses currently predominate in the United States, a new study published by CDC and partners highlights the comparative severity of illness associated with influenza A versus influenza B virus infections. The results of the study showed that among hospitalized adults, flu B viruses caused equally severe disease outcomes and clinical characteristics as flu A viruses.
This contradicts a common misconception that flu B viruses are associated with milder disease than flu A viruses.
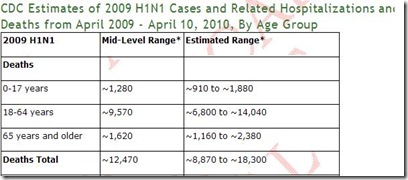
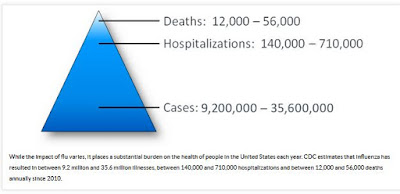
The study looked at the disease characteristics – including the severity of illness – associated with flu A and flu B viruses among hospitalized adults over eight flu seasons (2005-06 through 2012-13). The study identified 21,186 flu A and 3,579 flu B-associated hospitalizations during the study period. Flu A viruses were the predominant flu virus in circulation during all of the seasons studied, particularly during the 2009 H1N1 pandemic.
The study found no significant difference in the overall proportion of hospitalizations with an ICU admission by virus type for each season. Among hospitalized adults with flu A or B infection, length of hospital stay and the proportion of patients admitted into an Intensive Care Unit (ICU) were comparable. Results also showed that flu B virus infections caused a similar proportion of deaths as flu A virus infections among hospitalized adults during the study period.
Study findings prompted the authors to conclude that clinicians should not regard flu B infections as less severe than flu A when considering treatment options.
These findings support CDC’s existing antiviral treatment recommendations for the treatment of all hospitalized and high risk patients with suspected or confirmed flu infection. The type of flu virus infection (A or B) should not influence treatment decisions.
For most of the 2013-14 flu season, the 2009 H1N1 virus has been the predominant virus. However, over the past month and a half there has been a late season wave of flu B virus activity. At this time, flu B viruses are the predominant virus, with the highest levels of activity primarily focused in the Northeastern United States. Second waves of influenza B virus activity are not uncommon. About 70% of recent B viruses have been like the B virus component of the trivalent flu vaccine. The remaining flu B viruses have been like the second B vaccine component in the quadrivalent flu vaccine.
This study is available online from the Clinical Infectious Diseases journal website.
Interestingly, in last week's study NEJM: Acute Myocardial Infarction After Laboratory-Confirmed Influenza Infection, it was Influenza B (rather than A) that produced the highest coronary risk, at least among their limited sample size (n=364).
A finding that harkens back to the 2012 JID study mentioned above.It is a bit unusual to see influenza B dominated flu seasons in Asia and parts of Europe, since Influenza B generally peaks in the spring, after influenza A begins to wane. Some have suggested last summer's influenza A surge in Asia may have opened the door to a B-virus season.
This has been an interesting epidemiological twist, and one we'll want to learn more about.The good news is the flu shot (particularly the quadrivalent version) provides much better protection against influenza B viruses than we've seen in recent years against the A/H3N2 strain. With another 6 to 8 weeks of flu ahead, it isn't too late to get the shot.
Since influenza B viruses have only been found in humans and seals, they tend to evolve slowly, and are not viewed as serious pandemic threats. Nevertheless, they can spark large epidemics that produce significant morbidity and mortality.While old ideas about the severity of influenza B still persist, the evidence increasingly shows that influenza B viruses deserve the same respect as their A-list cousins.