|
| Original Map Credit Wikipedia |
#13,889
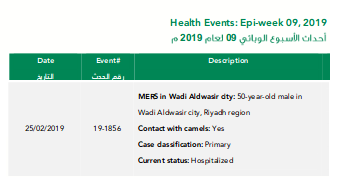
While the number of new cases continues to dwindle, today the Saudi MOH announced the 50th MERS case since January 29th in the relatively small (pop 106,000) town of Wadi Aldwasir, located about 500 km south of Riyadh.
Today's case involves a 50 y.o. male, hospitalized, listed as a primary case with recent camel contact.
Although it is very much a work in progress - with patient status updates being appended almost daily - below you'll find a current spreadsheet listing of the 50 Wadi Aldwasir cases.
Details are noticeably lacking, but from this list we can glean:
- 28 of 50 (56%) are listed as Secondary, Healthcare Acquired
- 7 cases (14%) are listed as Secondary, Household Contact but with no indication of how many households might be involved
- 13 of 50 cases (26%) are listed as Primary, community acquired
- Of those 8 had reported recent camel contact (direct or indirect)
- While 5 Primary community cases, appear to be without (or with uncertain) health facility or camel exposure
- 2 cases are listed as Secondary, Community-Acquired but without explanation as to how or where they occurred
While it is likely that most primary cases listed with recent camel contact became infected via that exposure, it is far from guaranteed. At least 5 of the cases attributed to household or healthcare transmission also reported recent camel contact.
But even assuming all of the primary cases listed as Camel contact are as described, we have 5 community-acquired cases (10%) that aren't attributed to a known exposure.Hospital and household clusters are well documented, but how and where these community acquired cases without an obvious risk exposure become infected remains one of the big unanswered questions about MERS.
The assumption is that some of these cases may be due to unidentified, mildly symptomatic (or asymptomatic) cases, who occasionally transmit the virus on to others in the community.
Last year, the WHO listed some of the `milder' symptoms that may be associated with MERS-CoV infection, including:
Low-grade fever, cough, malaise, rhinorrhoea, sore throat without any warning signs, such as shortness of breath or difficulty in breathing, increased respiratory (i.e. sputum or haemoptysis), gastro-intestinal symptoms such as nausea, vomiting, and/or diarrhoea and without changes in mental status (i.e. confusion, lethargy).While the jury is still out on how much of an infection risk an asymptomatic MERS patient poses, in recent years we've seen increasing evidence suggesting transmission to others is possible. Last December, we looked at:
Asymptomatic Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection: Extent and implications for infection control: A systematic review
Jaffar A.Al-Tawfiq abc Philippe Gautretd
Conclusions
The proportion of asymptomatic MERS cases were detected with increasing frequency as the disease progressed overtime. Those patients were less likely to have comorbid disease and may contribute to the transmission of the virus.
The good news thus far is - despite nagging questions over the sensitivity of current surveillance and the role of undetected cases in the spread of the disease - we've seen no signs of any sustained or efficient transmission of the MERS virus in the greater community.
The somewhat less-than-good-news is that the MERS virus continues to evolve, and may adapt more to a human host over time, and what we can say about its behavior now isn't guaranteed to last forever.