|
| Credit CDC |
#14,148
For the past 18 months we've been following the rising number of Hepatitis A infections across the nation, often (but not exclusively) reported among those who use injectable or non-injectable drugs, the homeless, and their close direct contacts. A few past blogs include:
CDC HAN Update: Vaccination Recommendations For Widespread Hepatitis A Outbreaks Across Multiple States
COCA Call On Multi-State Hepatitis A Outbreak
CDC HAN Advisory On Outbreak of Hepatitis A Virus (HAV) Infections among Drug Users & The Homeless - June 2018While Hepatitis A infection in a healthy adult usually results in a mild illness of a few week's duration - for some - particularly for those with compromised immune systems, it can be far more serious.
With the incidence of Hepatitis A rising across half the country, we've the latest surveillance numbers (as of June 21st) from the CDC.
Widespread outbreaks of hepatitis A across the United States
Since March 2017, CDC’s Division of Viral Hepatitis (DVH) has been assisting multiple state and local health departments with hepatitis A outbreaks, spread through person-to-person contact.
The hepatitis A vaccine is the best way to prevent HAV infection
The following groups are at highest risk for acquiring HAV infection or developing serious complications from HAV infection in these outbreaks and should be offered the hepatitis A vaccine in order to prevent or control an outbreak:People who use drugs (injection or non-injection)
One dose of single-antigen hepatitis A vaccine has been shown to control outbreaks of hepatitis A and provides up to 95% seroprotection in healthy individuals for up to 11 years.1,2
- People experiencing unstable housing or homelessness
- Men who have sex with men (MSM)
- People who are currently or were recently incarcerated
- People with chronic liver disease, including cirrhosis, hepatitis B, or hepatitis C
Pre-vaccination serologic testing is not required to administer hepatitis A vaccine. Vaccinations should not be postponed if vaccination history cannot be obtained or records are unavailable.
CDC has provided outbreak-specific considerations for hepatitis A vaccine administration.
 |
| Credit CDC |
 |
| Credit CDC |
CDC’s Response
In response to all hepatitis outbreaks, CDC provides ongoing epidemiology and laboratory support as well as support on vaccine supply and vaccine policy development. When requested, CDC sends “disease detectives” to affected areas to evaluate and assist in an outbreak response. CDC alerts other public health jurisdictions of any increases in disease. All jurisdictions are encouraged to be watchful for increases in hepatitis A cases. CDC also works with state and local health officials to ensure hepatitis A vaccine is targeted to the correct at-risk populations and that supply is adequate.
Admittedly this is a worrisome trend, but prior to the release of the first Hepatitis A vaccine in 1995, yearly numbers were far higher than we are seeing today.
From a 2005 JAMA report:
Incidence of Hepatitis A in the United States in the Era of Vaccination
Annemarie Wasley, ScD; Taraz Samandari, MD, PhD; Beth P. Bell, MD, MPH
National Trends in Hepatitis A Incidence
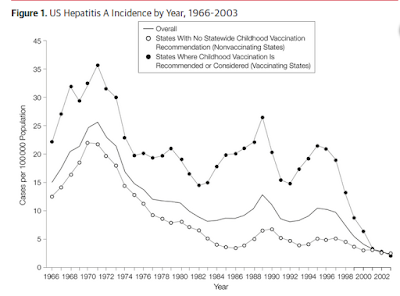
During the 35 years from 1966 through 1995, there were 2 cycles of hepatitis A incidence with peaks occurring in 1971 (59 000 cases; 29/100 000) and 1989 (36 000 cases; 14/100 000), and corresponding nadirs in 1983 (22 000 cases; 9.2/100 000) and 1992 (23 000 cases; 9.1/100 000) (Figure 1).
The CDC has advice for high risk individuals who should consider getting the vaccine at :
Frequently Asked Questions: Hepatitis A outbreaks
For the general public, however, the risks are pretty low. Still these outbreaks are another reminder why performing good hand hygiene should be a year-round practice, and not something reserved for flu season.