|
| Credit CDC |
#14,795
Although there is still much we don't know about the 2019 novel coronavirus - including its attack rate and overall severity - it is looking increasingly like 2019-nCoV could become a pandemic in the months ahead. The virus appears to transmit readily in humans, and the number of cases outside of China are likely to climb rapidly.
Pandemics come in all sizes and shapes, and can range from severe (1918), to moderate (1957), to relatively mild (2009). But regardless of its overall severity, history tells us most people who will be infected are likely to only have mild to moderate illness.As hospitals only have a limited number of beds and staff to care for patients, once a certain threshold of cases appears in any country or region, hospitals will only be able to admit and treat those who are most severely ill.
Patients with mild or moderate illness - who can likely recover without medical intervention - will need to be treated at home.The CDC, in anticipation of all of this, is generating interim guidance based on past experiences with SARS-Cov and MERS-CoV, for a broad range of venues and topics. While home patient care is likely going to be little different than for influenza (see CDC Flu Homecare), it is important to limit the spread (and impact) of a pandemic virus within the home, and in the greater community.
To that end, the CDC published the following guidance on February 1st, on how to limit the spread of 2019-nCov. I'll have a brief postscript after the break.
Interim guidance for persons who may have 2019 Novel Coronavirus (2019-nCoV) to prevent spread in homes and residential communities
Simplified Chinese Translation
February 1, 2020
This interim guidance is based on what is currently known about the epidemiology of 2019-nCoV and the transmission of other viral respiratory infections. CDC will update this interim guidance as needed and as additional information becomes available.
Coronaviruses are a large family of viruses, some causing illness in people and others that circulate among animals, including camels, cats, and bats. Rarely, animal coronaviruses can infect people exposed to infected animals, and then spread among people, as has been seen with MERS-CoV and SARS-CoV, and now 2019-nCoV. This interim guidance may help prevent this virus from spreading among people in their homes and in other residential communities.
This interim guidance is intended for:
Below are Preventative Steps for
- People with confirmed or suspected 2019-nCoV infection, including patients under investigation, who do not need to be hospitalized and who can receive care at home (see Interim Guidance for Implementing Home Care of People Not Requiring Hospitalization for 2019 Novel Coronavirus (2019-nCoV));
- People with confirmed 2019-nCoV infection, who were hospitalized, determined to be medically stable, and discharged home (see Interim Guidance for Implementing Home Care of People Not Requiring Hospitalization for 2019 Novel Coronavirus (2019-nCoV));
- Other people who have had close contact with a person with confirmed 2019-nCoV infection.
People with confirmed or suspected 2019-nCoV infection (including patients under investigation) who do not need to be hospitalized
and
People with confirmed 2019-nCoV infection who were hospitalized and determined to be medically stable to go home
Your doctors and public health staff will evaluate whether you can be cared for at home. If it is determined that you do not need to be hospitalized and can be isolated at home, you will be monitored by staff from your local or state health department. You should follow the prevention steps below until a healthcare provider or local or state health department says you can return to your normal activities.
Stay home except to get medical care
You should restrict activities outside your home, except for getting medical care. Do not go to work, school, or public areas. Do not use public transportation, ride-sharing, or taxis.
Separate yourself from other people in your home
As much as possible, you should stay in a specific room and away from other people in your home. Also, you should use a separate bathroom, if available.
Call ahead before visiting your doctor
If you have a medical appointment, call the healthcare provider and tell them that you have or may have 2019-nCoV infection. This will help the healthcare provider’s office take steps to keep other people from getting infected or exposed.
Wear a facemask
You should wear a facemask when you are around other people (e.g., sharing a room or vehicle) and before you enter a healthcare provider’s office. If you are not able to wear a facemask (for example, because it causes trouble breathing), then people who live with you should not stay in the same room with you, or they should wear a facemask if they enter your room.
Cover your coughs and sneezes
Cover your mouth and nose with a tissue when you cough or sneeze. Throw used tissues in a lined trash can and wash your hands with soap and water for at least 20 seconds. If soap and water are not available, immediately clean your hands with an alcohol-based hand sanitizer that contains at least 60% alcohol, covering all surfaces of your hands and rubbing them together until they feel dry. Soap and water should be used preferentially if hands are visibly dirty.
Clean your hands
Wash your hands often with soap and water for at least 20 seconds. If soap and water are not available, clean your hands with an alcohol-based hand sanitizer that contains at least 60% alcohol, covering all surfaces of your hands and rubbing them together until they feel dry. Soap and water should be used preferentially if hands are visibly dirty. Avoid touching your eyes, nose, and mouth with unwashed hands.
Avoid sharing personal household items
You should not share dishes, drinking glasses, cups, eating utensils, towels, or bedding with other people in your home. After using these items, they should be washed thoroughly with soap and water.
Monitor your symptoms
Seek prompt medical attention if your illness is worsening (e.g., shortness of breath or difficulty breathing). Before seeking care, call your healthcare provider and tell them that you have, or are being evaluated for, 2019-nCoV infection. Put on a facemask before you enter the facility. These steps will help the healthcare provider’s office to keep other people from getting infected or exposed. Ask your healthcare provider to call the local or state health department. Persons who are placed under active monitoring or facilitated self-monitoring should follow instructions provided by their local health department or occupational health professionals, as appropriate.
Discontinuing home isolation
Patients with confirmed 2019-nCoV infection should remain under home isolation precautions until the risk of secondary transmission to others is thought to be low. The decision to discontinue home isolation precautions should be made on a case-by-case basis, in consultation with healthcare providers and state and local health departments. Current information on 2019-nCoV is limited; thus, home precautions are conservative and based on general recommendations for other coronaviruses, like Middle Eastern Respiratory Syndrome (MERS).
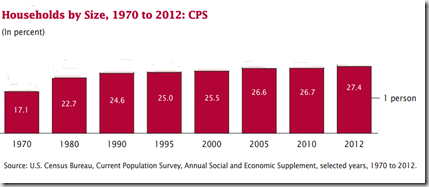
Like many Americans, I live alone. It is a demographic trend that has been increasing for decades. In 2012 the Census bureau reported that 1 in 4 households had just a single occupant - greater than at any time in the past century.
Currently, more than 32 million Americans live alone (see chart below), and while many of those are younger people who are waiting later to get married, a side effect of our longer lifespan and high divorce rate is that many of these single households are held by those over the age of 65.
Whether we live alone by choice or by happenstance, we all share a common vulnerability. If we get sick, or injured, there may be no one around to notice, or to help.
As a paramedic I saw a number of people who lived alone who either died, or spend miserable hours or even days incapacitated and unable to call for help, due to an illness or accident.Another vulnerable group are households with only 1 adult, and minor children. This too is a growing demographic, with more than 5 million households falling into that category. If the lone adult falls seriously ill, then even more lives are potentially at risk.
Because of a bad bout of flu I experienced in 2007, I began to promote the idea of having – and being – a `flu buddy’ about a dozen years ago in this blog. Particularly for those who either live alone, or are the sole adult caregiver in a household.
A `Flu buddy’ is simply someone you can call if you get sick, who will then check on you every day (in person, by phone, social media, etc.) , make sure you have the medicines or food you need, help care for you if needed, and who can call for medical help if your condition deteriorates.Something as simple as dehydration from a fever, or being too weak (or stubborn) to call for help, can be deadly in what would otherwise be a manageable illness. Having and/or being a flu buddy can remedy that and save lives.
After the 2009 H1N1 pandemic, I expanded the idea into becoming and being a `Disaster Buddy', to cover more than illness (see In An Emergency, Who Has Your Back?).
Now is the time to sit down and openly discuss with family, neighbors, and friends how you will backstop one another during an emergency, whether it be a hurricane, an earthquake, a flood, or a pandemic.Because we can all get through any crisis a lot better with a little help from our friends.