#16,922
Yesterday, in More Evidence On The Long-term Impact of SARS-CoV-2 Infection, we looked at neurological and cardiovascular impacts - mostly in adults - linked to prior COVID infection.
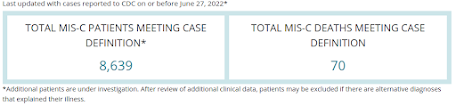
Children and adolescents - while generally less severely affected by COVID - are not immune to serious illness, as we've seen from thousands of reports of multisystem inflammatory syndrome in children (MIS-C) across the nation, and around the world.
- The median age of patients with MIS-C was 9 years. Half of children with MIS-C were between the ages of 5 and 13 years.
- 57% of the reported patients with race/ethnicity information available (N=8,143) occurred in children who are Hispanic/Latino (2,145 patients) or Black, Non-Hispanic (2,489 patients).
- 98% of patients had a positive test result for SARS CoV-2, the virus that causes COVID-19. The remaining 2% of patients had contact with someone with COVID-19.
- 61% of reported patients were male.
MIS-C isn't the only adverse outcome for children and adolescents with COVID.
Last January the MMWR reported on increased risk among those 18 and younger of developing diabetes within 30 days of COVID infection, and we've seen studies indicating elevated rates of COVID-19–Associated Pulmonary Embolism in Pediatric Patients.
The American Academy of Pediatrics maintains a web page devoted to Post-COVID Conditions in Children and Teens, and the CDC reported in a recent slide presentation:
Post–COVID-19 Symptoms and Conditions Among Children and Adolescents — United States, March 1, 2020–January 31, 2022
Weekly / August 5, 2022 / 71(31);993–999
Lyudmyla Kompaniyets, PhD1; Lara Bull-Otterson, PhD1; Tegan K. Boehmer, PhD1; Sarah Baca1,2; Pablo Alvarez, MPH1,2; Kai Hong, PhD1; Joy Hsu, MD1; Aaron M. Harris, MD1; Adi V. Gundlapalli, MD, PhD1; Sharon Saydah, PhD1 (View author affiliations)View suggested citation
Summary
What is already known about this topic?
Children and adolescents might be at risk for certain post-COVID symptoms and conditions.
What is added by this report?
Compared with patients aged 0–17 years without previous COVID-19, those with previous COVID-19 had higher rates of acute pulmonary embolism (adjusted hazard ratio = 2.01), myocarditis and cardiomyopathy (1.99), venous thromboembolic event (1.87), acute and unspecified renal failure (1.32), and type 1 diabetes (1.23), all of which were rare or uncommon in this study population.
What are the implications for public health practice?
COVID-19 prevention strategies, including vaccination for all eligible persons aged ≥6 months, are critical to preventing SARS-CoV-2 infection and subsequent illness, and reducing the public health impact of post-COVID symptoms and conditions among persons aged 0–17 years.
PDF [312K]
Post–COVID-19 (post-COVID) symptoms and conditions* are new, recurring, or ongoing health problems that occur 4 or more weeks after infection with SARS-CoV-2 (the virus that causes COVID-19). Previous studies have characterized and estimated the incidence of post-COVID conditions among adults (1,2), but data among children and adolescents are limited (3–8).Using a large medical claims database, CDC assessed nine potential post-COVID signs and symptoms (symptoms) and 15 potential post-COVID conditions among 781,419 U.S. children and adolescents aged 0–17 years with laboratory-confirmed COVID-19 (patients with COVID-19) compared with 2,344,257 U.S. children and adolescents without recognized COVID-19 (patients without COVID-19) during March 1, 2020–January 31, 2022. The analysis identified several symptoms and conditions with elevated adjusted hazard ratios among patients with COVID-19 (compared with those without).The highest hazard ratios were recorded for acute pulmonary embolism (adjusted hazard ratio [aHR] = 2.01), myocarditis and cardiomyopathy (1.99), venous thromboembolic event (1.87), acute and unspecified renal failure (1.32), and type 1 diabetes (1.23), all of which were rare or uncommon in this study population.Conversely, symptoms and conditions that were most common in this study population had lower aHRs (near or below 1.0). Patients with COVID-19 were less likely than were patients without to experience respiratory signs and symptoms, symptoms of mental conditions, muscle disorders, neurological conditions, anxiety and fear-related disorders, mood disorders, and sleeping disorders. COVID-19 prevention strategies, including vaccination for all eligible children and adolescents, are critical to prevent SARS-CoV-2 infection and subsequent illness, including post-COVID symptoms and conditions (9).(SNIP)
The findings in this report are subject to at least seven limitations.
- First, the definitions of potential post-COVID symptoms and conditions are subject to misclassification bias because the symptoms and conditions were defined by a single ICD-10-CM code and no information on laboratory assessments or degree of severity was available.
- Second, because the incidence date of a symptom or a condition was based on the first occurrence of the ICD-10-CM code, the actual incidence date of that symptom or condition might have occurred prior to COVID-19.
- Third, patients infected with SARS-CoV-2 without a documented COVID-19 diagnosis or positive test result might have been misclassified as not having had COVID-19, potentially reducing the magnitude of observed associations.
- Fourth, the aHR estimates might be reduced because patients without COVID-19 were patients with a health care encounter possibly related to COVID-19.
- Fifth, because patients’ vaccination status was likely underreported in this dataset, this analysis was not adjusted for previous receipt of COVID-19 vaccines.
- Sixth, although this study relied on statistical significance for interpreting the increased rates of symptoms and conditions, further understanding of the clinical significance of the observed associations, including whether these symptoms and conditions are transient or chronic, is necessary.
- Finally, generalizability might be limited because the analysis was restricted to children and adolescents aged 0–17 years included in a medical claims database, approximately 70% of whom were enrolled in Medicaid managed care; therefore, findings are not necessarily representative of all children and adolescents with COVID-19 or of those who do not seek health care.
These findings can be used to apprise health care professionals and caregivers about new symptoms and conditions that occur among children and adolescents in the months after SARS-CoV-2 infection. COVID-19 prevention strategies, including vaccination for all eligible persons aged ≥6 months, are critical for preventing SARS-CoV-2 infection and subsequent illness and for reducing the public health impact of post-COVID symptoms and conditions.