https://www.cdc.gov/flu/pdf/avianflu/avian-flu-transmission.pdf
#17,313
The revelation yesterday from the Cambodian CDC that this week's family cluster of H5N1 was From Clade 2.3.2.1c - and not from clade 2.3.4.4b which is currently circulating in Europe and North America - is both a relief and a renewed concern.
While everyone can be heartened by the fact that this fatal case/family cluster was not sparked by the same bird flu virus which is currently in our own backyard, it is a reminder that some of the older, more dangerous H5N1 clades still exist in the wild, and pose a threat.
Yesterday the CDC released a statement on the two Cambodian cases, along with an excellent timeline of avian flu events since 2020.
H5N1 Update: Two Human H5N1 Cases in Cambodia
February 25, 2023 — Two human infections with avian influenza A H5N1 (H5N1 bird flu) have been reported by Cambodia. These cases are thought to be a result of exposure to infected birds/poultry. An investigation to try to confirm the source of the infections and detect any potential additional cases is ongoing. Based on preliminary genetic sequencing done in country, the Cambodian Ministry of Health has identified these viruses as being H5 clade 2.3.2.1c, which have circulated in Cambodia among birds/poultry for many years. These viruses have resulted in rare sporadic human infections in the past, but these two cases are the first such infections reported in Cambodia since 2014. The 2.3.2.1c viruses in Cambodia are different from H5N1 viruses currently circulating in wild birds and poultry in the United States and other countries, which are H5 clade 2.3.4.4b.
The cases in Cambodia occurred in a child, who died, and her father, who reported a fever and cough. No additional H5N1 cases have been identified at this time. To date, no indication of person-to-person spread has been found. There is no indication at this time that these two human cases of H5N1 in Cambodia pose a threat to the U.S. public.
What CDC is Doing
The Cambodian Ministry of Health and other global public health officials are leading the investigation into these two human cases with support from in-country CDC staff and a CDC rapid response team. Investigation efforts include contact tracing, monitoring and/or testing of close contacts including health care workers who cared for the two patients, and testing of animals in the village. CDC also is providing testing materials and reagents. CDC will continue to work with the Cambodian Ministry of Health and will provide updates as needed.
Risk and Prevention Measures in the U.S.
For the United States, the ongoing outbreaks of 2.3.4.4b clade H5N1 bird flu in wild birds and poultry with sporadic spillover events into some mammals remains mainly an agricultural issue. The current risk to the general public from bird flu viruses remains low; however, it is important to remember that risk depends on exposure, and people with more exposure might have a greater risk of infection. People who have job-related or recreational exposures to infected birds or sick or dead mammals are at higher risk of infection and should take appropriate prevention measures. CDC also has guidance for clinicians on monitoring, testing, and antiviral treatment for patients with bird flu virus infections.
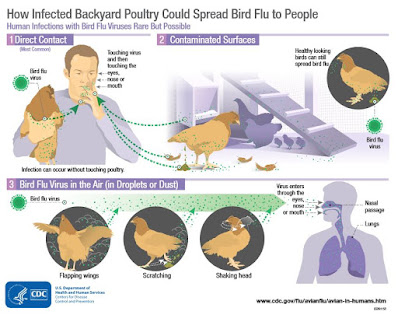
People should avoid contact with poultry, and wild birds and mammals that appear ill or are dead and avoid contact with surfaces that appear to be contaminated with feces from wild birds and mammals, or domestic poultry. Observe wild birds and mammals only from a distance, if possible. Wild birds and mammals can be infected with bird flu viruses without always appearing sick. If you must handle wild birds and mammals or sick or dead poultry, minimize direct contact by wearing gloves and wash your hands with soap and water after touching them. If available, wear respiratory protection such as a medical facemask and eye protection such as goggles.
The U.S. poultry industry has strict health and safety standards, including regular monitoring for bird flu. It is safe to eat properly handled and cooked poultry and poultry products in the U.S. The proper handling and cooking of poultry and eggs to an internal temperature of 165˚F kills bacteria and viruses, including H5 viruses.
The U.S. Department of Interior and USDA APHIS are the lead federal agencies for H5N1 in birds, poultry, and animals in the U.S. They are respectively responsible for outbreak investigation and control of bird flu in wild birds and in domestic poultry. CDC is the lead federal agency on the human health side.
CDC has been actively working on the domestic H5N1 situation since the initial detection of H5N1 in U.S. wild birds and poultry in early 2022. This includes preparing for the possibility that H5N1 viruses circulating in birds in the United States and in other countries gain the ability to easily infect and spread between people. This includes ensuring that there are prevention and treatment tools, in addition to testing capacity.
CDC’s existing influenza surveillance systems are well-equipped to rapidly detect cases of avian influenza A virus infection, including H5N1 virus, in people. CDC’s influenza virus tests, which can detect both seasonal and novel influenza A viruses, are used in all 50 U.S states and globally. Additionally, there are CDC diagnostic tests that specifically detect the current H5 viruses, which are available in public health laboratories in all 50 U.S. states and international laboratories.
An H5 candidate vaccine virus (CVV) produced by CDC is identical or nearly identical to the hemagglutinin (HA) protein of recently detected clade 2.3.4.4b H5N1 viruses in birds and mammals (including a 2022 H5 outbreak in mink in Spain) and could be used to produce a vaccine for people, if needed, and which would provide good protection. This H5 CVV is available and has been shared with vaccine manufacturers. Because flu viruses are constantly changing, CDC continually analyses viruses to identify genetic changes that suggest these viruses might spread more easily to and between people, and cause serious illness in people, or for changes that suggest reduced susceptibility to antivirals, as well as changes in the virus that might mean a new vaccine virus should be developed.
CDC, along with state and local public health partners, also continues to actively monitor people who have been exposed to infected birds and poultry for 10 days after exposure. To date, public health departments have monitored more than 6,300 people in more than 50 jurisdictions who were exposed to birds/poultry infected with H5N1 virus. Of these, more than 160 people showed symptoms and subsequently were tested for novel influenza A and seasonal flu viruses along with other respiratory viruses. H5N1 virus genetic material has been only detected in a respiratory specimen from one person in Colorado.
Additional information on protective actions around birds, including what to do if you find a dead bird, is available. CDC also has guidance for specific groups of people with exposure to poultry, including poultry workers and people responding to poultry outbreaks. CDC will continue to provide further updates to the situation and update guidance as needed.
Human infections with avian influenza viruses are rare but can happen following exposure to infected birds/poultry. Even more rarely, some limited, non-sustained person-to-person spread has happened. More information about avian influenza is available on the CDC website.
And that could happen again.
But influenza's superpower lies in its ability to evolve, adapt, and reinvent itself (via reassortment).
Which means we can't count it out simply because it hasn't stumbled upon the right combination of mammalian adaptations yet. And if H5N1 ultimately fails, there is a long list of other novel viruses which pose credible public health threats.
Stay tuned.