#18,189
While we saw a lot of pandemic preparedness in the first decade of the 21st century, the practice fell out of favor following the relatively `mild' 2009 H1N1 pandemic, and many countries continue to work with nearly 20-year-old plans.
As a result, the world was caught flat-footed and largely unprepared for the COVID pandemic of 2020, and in many cases, surveillance and reporting today are arguably less robust than they were 5 years ago (see No News Is . . . Now Commonplace).
A little less than a month ago, South Korea's CDC released a Revised ‘Influenza Pandemic Preparedness and Response Plan’, and we've seen recent calls from the WHO and from the ECDC to member nations to increase surveillance and preparedness.
These guidelines run well over 100 pages (all in Japanese), and the 5-page summary document I found (and translated) was pretty vague.
I expect additional details will emerge in the days ahead.
Summary of Proceedings
議事要旨[PDF形式:780KB]
Guidelines for the Government Action Plan for Countermeasures against Novel Influenza and Other Pandemics (Draft)
[Document 1] Guidelines for information gathering and analysis [850KB]

[Document 2] Guidelines for surveillance [330KB]

[Document 3] Guidelines for information provision and sharing, and risk communication [281KB]

[Document 4] Guidelines for border control measures [237KB]

[Document 5] Guidelines for prevention of spread [1.1MB]

[Document 6] Guidelines for vaccinations (vaccines) [471KB]

[Document 7] Guidelines for medical care [564KB]

[Document 8] Guidelines for therapeutic drugs and treatment methods [298KB]

[Document 9] Guidelines for testing [429KB]

[Document 10] Guidelines for health [275KB]

[Document 11] Guidelines for securing supplies [193KB]

[Document 12] Guidelines for measures against new strains of influenza, etc. for businesses and workplaces [293KB]

[Document 13] Guidelines for smooth implementation of burials and cremations [125KB]
From [Document 5] Guidelines for prevention of spread [1.1MB] 
(1) Basic Concept of Measures to Prevent the Spread of Influenza
The purpose is to prevent the spread of influenza as much as possible, to minimize the damage to health, and to minimize the impact on people's lives and socio-economic activities.
In addition to providing appropriate medical care, it is important to take measures to prevent the spread of infection as necessary to prevent the spread of infection and to keep the speed and peak of the spread of infection and the number of patients requiring treatment within the range that the medical care system can handle. In particular, when there are no effective treatments or until vaccinations are available, prevention measures implemented from a public health perspective are important.
For this reason, risk assessments based on the characteristics of the pathogen (pathogenicity, infectivity, drug susceptibility, etc.) will be conducted in a timely and appropriate manner, and if there is a risk of a large-scale spread of infection that would overwhelm medical care even in an enhanced medical care system, measures to prevent the spread of infection, including priority measures to prevent the spread of new influenza, etc. (hereinafter referred to as "priority measures to prevent the spread") and emergency measures for new influenza, etc. (hereinafter referred to as "emergency measures") based on the Special Measures Act for Countermeasures against Novel Influenza, etc. (Act No. 31 of 2012, hereinafter referred to as the "Special Measures Act"), will be taken promptly for the areas, period, and targets considered necessary.
On the other hand, Article 5 of the Special Measures Act stipulates that if restrictions are imposed on the freedom and rights of citizens, such restrictions shall be the minimum necessary to implement measures against novel influenza, etc. In addition, measures to prevent the spread of infection have a significant impact on socio-economic activities, and in particular, when measures are taken against patients and close contacts, the burden on those involved in the measures, such as public health center staff, is heavy.
In light of this, it is important to consider the effectiveness and impact of measures in a comprehensive manner and to consider taking necessary measures to prevent the spread of infection. It is also important to review measures being implemented flexibly and promptly, such as reducing or suspending measures, in response to changes in the situation, such as information on the characteristics of infectious diseases and the properties of pathogens (pathogenicity, infectivity, drug susceptibility, etc.) and the development and dissemination of vaccines and treatments.
The above graphic is essentially the `flattening the curve' strategy (see below) which has long been part of the U.S. pandemic plan, to reduce a pandemic's impact on limited healthcare resources and essential workers.
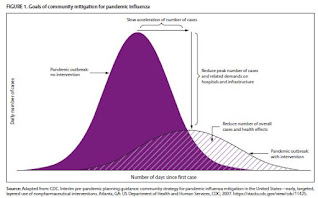 |
| Flattening the Curve - Credit CDC |
While No Pandemic Plan Survives Contact With A Novel Virus, it is still vital to have a plan going into any crisis. The following quote is nearly 20 years old, but it is just as true today as it was in 2006:
“Everything you say in advance of a pandemic seems alarmist. Anything you’ve done after it starts is inadequate." - Michael Leavitt, Former Secretary of HHS
Hopefully other countries are updating their own plans as well.

