#18,540
As we've discussed often over the years, there are a lot of H5Nx viruses in the wild, with some being far more pathogenic (in birds, or in mammals) than others (see 2012's Differences In Virulence Between Closely Related H5N1 Strains).
Over the past 2 years Cambodia has reported 18 human H5N1 infections (clade 2.3.2.1c), with nearly a 40% fatality rate, while roughly half of the reported H5N6 infections in China over the past decade have succumbed to the infection.
In sharp contrast, the United States has confirmed 66 human infections with H5N1 over the past 10 months, with just one fatality. While somewhat reassuring, there are no guarantees that this kinder-and-gentler variant will remain dominant.
So far in 2024, three notable genotypes have emerged:
- B3.13 aka the `bovine' strain affecting dairy cattle in at least 16 states and mildly infecting dozens of humans
- D1.1 a wild bird/poultry strain which has spilled over into > a dozen people in Washington State, severely infected a teenager in British Columbia, and produced a fatal infection in Louisiana.
- D1.2 a wild bird/poultry strain which recently detected in poultry and 2 pigs in Oregon
That said, more than 100 genotypes of H5N1 have been reported in North America since the H5 virus arrived in late 2021, and more are expected to emerge over time.
Last August, we looked at a preprint by NIAID researchers at the NIH facility in Hamilton, MT, which found the bovine B3.13 genotype doesn't replicate in human lung tissues as well - or produce as strong of an immune response - as an earlier, more pathogenic, H5N1 strain (A/Vietnam/1203/2004).
Note: This study predates the emergence of the D1.1 and D1.2 genotypes.
Their peer reviewed dispatch was published this week in the CDC's EID Journal (see below). Due to its length, I've only preproduced the abstract and some excerpts.
Follow the link to read it in its entirety. I'll have a brief postscript when you return.
Dispatch
Meaghan Flagg1, Brandi N. Williamson1, Johan A. Ortiz-Morales, Tessa R. Lutterman, and Emmie de WitComments to Author
Author affiliation: National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA
Abstract
We compared virus replication and host responses in human alveolar epithelium infected with highly pathogenic avian influenza (HPAI) A(H5N1) viruses. A/Vietnam/1203/2004 replicated most efficiently, followed by A/Texas/37/2024, then A/bovine/Ohio/B24OSU-342/2024. Induction of interferon-stimulated genes was lower with A/Texas/37/2024 and A/bovine/Ohio/B24OSU-342/2024, which may indicate a reduced disease severity of those viruses.
(SNIP)
The unusual transmission of clade 2.3.4.4b HPAI H5N1 viruses to mammals has raised concerns about the risk for spillover into the human population, and the possibility of outbreaks leading to severe disease. We assessed virus replication and host responses in human alveolar epithelium because virus replication and host cell damage in that site is a key driver of severe respiratory disease.
The reduced replication levels of the contemporary A/Texas/37/2024 and A/bovine/Ohio/B24OSU-342/2024 isolates in lung organoids compared with the historic A/Vietnam/1203/2004 isolate could explain why recent human influenza cases involving the clade 2.3.4.4b viruses resulted in mild illness (4,6), as opposed to the severe respiratory disease associated with previous HPAI outbreaks in Vietnam (13,14).
The presence of a lysine at position 627 in the polymerase basic (PB) 2 protein has been associated with adaption of avian influenza viruses to mammal hosts and is known to increase virus replication in the mammalian respiratory tract (15). That substitution (E627K) is in both the A/Vietnam/1203/2004 and A/Texas/37/2024 viruses but not the A/bovine/Ohio/B24OSU-342/2024 isolate (4), which could explain the increased replication observed for the A/Texas/37/2024 isolate compared with the bovine isolate.
Another factor contributing to the reduced disease severity in humans after infection with clade 2.3.4.4b viruses compared with previous HPAI H5N1 virus cases may be differential activation of the immune system.
We observed substantially higher induction of ISGs in lung organoids infected with the A/Vietnam/1203/2004 isolate. An overly exuberant immune response, including cytokine storm, is known to play a role in the high mortality rates from HPAI H5N1 virus infections observed during the 2003 and 2004 outbreaks in Vietnam (14). Reduced ISG induction elicited by the A/Texas/37/2024 and A/bovine/Ohio/B24OSU-342/2024 isolates despite detection of virus replication might indicate that those viruses have further adapted to counteract the interferon system in humans, possibly due to their more extensive circulation in mammals. That limited innate immune activation may contribute to their reduced pathogenicity along with other factors, such as differences in prior immunity.
Despite differences in virus replication and ISG induction, we observed similar levels of cell death by 96 hours postinoculation for all 3 viruses. Previous work has shown that direct virus-induced cytotoxicity is not always indicative of pathogenicity in vivo because cytotoxicity was not observed in SARS-CoV-2–infected lung organoids (11), despite the ability of that virus to cause severe respiratory disease. Taken together, those data suggest that epithelial-extrinsic factors, possibly related to immune activation, govern pathogenicity in vivo.
Conclusions
In summary, this study provides a characterization of virus replication and host responses to infection in human alveolar epithelium between a contemporary clade 2.3.4.4b human HPAI H5N1 isolate and the highly virulent A/Vietnam/1203/2004 virus. Further studies are warranted to understand how these viruses interact with the innate immune system, particularly regarding differential ISG and proinflammatory cytokine induction, and how this affects pathogenesis in vivo.
Nonetheless, our results indicate that the clade 2.3.4.4b HPAI viruses currently circulating in cattle will likely exhibit reduced human disease severity compared with historic HPAI viruses but should be closely monitored for changes that may influence pathogenicity or transmissibility.
Dr. Flagg is a postdoctoral fellow in the Molecular Pathogenesis Section of the Laboratory of Virology, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health. Her primary interests are epithelial stem cell biology and repair during virus infection.
While the B3.13 genotype currently appears poorly suited to spark a major outbreak in humans, that could change. It's persistence and spread in cattle - and continued spillover into humans, cats, birds, and other mammals - provides it with numerous opportunities to evolve and adapt into something more formidable.
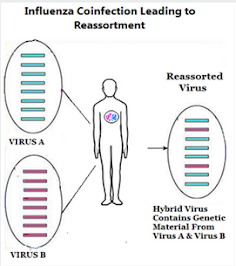
A `mild' H5 infection in a farmworker - who happens to be simultaneously infected with a `seasonal flu' - could yield a reassortant with unpredictable capabilities.
And if B3.13 is truly a dead end, then D1.1, D1.2, or some other genotype (anywhere in the world) could easily take center stage in the weeks and months ahead.
And if it turns out that HPAI H5 doesn't have the `right stuff' to start a pandemic, there are dozens of other subtypes (H1,H2,H3,H7,H9,H10, etc.) in the wild that can give it a go.
Making another pandemic only a matter of when, not `if'.