
King Fahd Hospital ER – Credit http://riyadhconnect.com
# 8557
Over the past 6 weeks we’ve seen a surge in MERS cases, particularly associated with healthcare facilities in Saudi Arabia and the UAE, and infecting a large number of healthcare workers. Although we’ve seen photographic evidence that HCWs in Saudi Arabia often wear surgical masks (see above), less often do we see doctors and nurses wearing eye protection.
Today, Egyptian cardiologist and board member of their Medical Association, Dr. Khaled Samir, is quoted as saying he believes the reason so many HCWs have been infected is that the virus enters the body through the eyes, and that proper PPEs (Personal Protective Equipment) are in short supply.
First, some excerpts from the news report, then I’ll be back with a bit more on transocular transmission of viruses. This from Egyptnews.org.
Dr. Khaled Samir: doctors are more susceptible to the "Corona"
May 2, 2014 in
Said Dr. Khaled Samir cardiologist, chest and treasurer of the Medical Association, said there are many ways to infection with "Corona" flu-like regular, Katts or use tools infected with the virus or the lack of attention to personal hygiene, pointing out that the way the infection most dangerous virus "Corona", is that it may transmitted from person to person through the'' eye''.
Samir added, in a press statement, said Friday that there are special types of masks'''' should be used with this type of infection, expressing regret at the lack of these masks in Egypt, despite the availability of other countries and the use of her doctors with all cases of infection.
The doctor explained that the catcher normal is not a matter of how to prevent transmission of the virus, stressing that it should at least use the mask of anti-virus and wear glasses certain resemble glasses sea, to prevent the doctor himself from infection during the examination of patients suspected of having the "Corona."
While transocular infection from the MERS virus hasn’t been documented, we do know that other respiratory viruses – such as the H7 avian flu virus and the 2009 H1N1pdm virus – have demonstrated an affinity for the tissues of the eye, and can present with conjunctivitis (see I Only Have Eyes For Flu).
In Ocular Tropism of Respiratory Viruses by Belser, Rota & Tumpey, the authors write:
While species D adenoviruses and subtype H7 influenza viruses are known to possess an ocular tropism, documented human ocular disease has been reported following infection with all principal respiratory viruses.
Ocular tropism isn’t the only route to infection through the eyes, as there is a physical bridge as well.
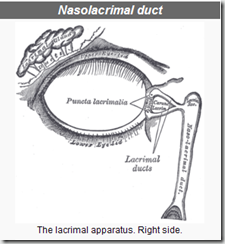
The nasolacrimal system contains a duct that drains the lacrimal gland in the eye into the nasal cavity. This shortcut to the upper respiratory system is why you can sometimes taste eye drops, and can easily circumvent the protective barrier of a facemask.
Credit Wikipedia
While aerosolized or droplet transmission to the eyes is certainly possible, we also (usually, unconsciously) touch our face and eyes dozens of times each hour, and that could also introduce the virus into the eyes, picked up from contaminated surfaces or fomites.
For HCWs dealing with MERS, the CDC strongly recommends wearing a fit-tested N95 mask, eye protection, gown & gloves (see Survival Of The Fit-tested). The World Health Organization’s recommended infection control guidelines are not quite as exacting (no doubt due to the wide disparity of resources available among nations), but nonetheless recommend eye protection .
For the past couple of months the WHO has included this reminder in every MERS update (bolding mine):
Droplet precautions should be added to the standard precautions when providing care to all patients with symptoms of acute respiratory infection. Contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS-CoV infection. Airborne precautions should be applied when performing aerosol generating procedures.
Over the past few years the transocular route of viral infection has become more evident, and in 2011 we looked at some intriguing research on the relative efficacy of wearing a mask vs. wearing a mask & eye protection (see PPEs & Transocular Influenza Transmission).
Researchers at Wake Forrest chose to expose 28 volunteers (divided into six groups) for 20 minutes to an aerosolized LAIV (Live Attenuated Influenza Vaccine) in a special air-tight chamber.
The six groups were:
- No protective equipment
- Ocular exposure only
- Surgical mask only
- Surgical mask plus eye protection
- Fit-tested N-95 only
- Fit-tested N-95 plus eye protection
- Researchers detected flu virus in all 4 subjects in Group 1 (unprotected), and in 3 of 4 in Group 2 (Ocular Exposure only).
- Somewhat surprisingly, nasal washes of subjects with ocular exposure only were positive for flu virus within 30 minutes, suggesting the virus made its way rapidly to the nasopharynx by way of the nasolacrimal duct.
- Flu virus was detected in all 10 volunteers who wore surgical masks (groups 3 & 4), regardless of eye protection.
- N95 wearers (group 5) fared somewhat better, with 3 of 5 testing positive for the virus.
- The best result came from the wearing of eye protection and an N95 (group 6). Only 1 in 5 subjects wearing that combination of protection showed detectable levels of virus.
The authors conclude:
"The eyes could be an entry route for influenza, allowing viral particles easy and fast access to the upper respiratory tract.
The type of surgical mask tested was inferior to a fit-tested N95 respirator in preventing aerosol delivery; however, none of the tested barrier precautions provided complete protection, including a CDC-recommended fit-tested N95 respirator and the addition of eye protection.”
Granted, the MERS coronavirus isn’t influenza, and right now we don’t have any direct evidence that it can be efficiently transmitted via the transocular route. But the notion of transocular transmission would at least seem plausible.
And if there have been lapses in the use of eye protection – as suggested by some of the the photos posted online, and Dr. Samir – then this might play some part in the high rate of infection among healthcare workers.
Questions that can only really be answered by some good old fashioned gumshoe epidemiology. But hopefully questions that will be answered sooner than later.