# 9693
Joining the parade of recently published summaries and risks assessments on the MERS Coronavirus (see ECDC: Updated Rapid Risk Assessment On MERS-CoV & MMWR: MERS Epidemiological Update & Guidance), the World Health Organization has published a 10-page review of MERS cases, recent publications, and the risk assessment.
As before, they find both zoonotic transmission and nosocomial outbreaks to contribute to the ongoing stream of cases, as noted by WHO spokesperson Gregory Hartl on twitter earlier this morning.
While you’ll no doubt want to download and read the entire PDF file, I’ve excerpted a few passages below.
(EXCERPTS)
Summary and Risk Assessment
WHO is continuing to work with Ministries of Health in affected countries and with international partners to better understand the reasons for the increase in cases reported in the Spring of 2014. As previously reported, WHO/GOARN missions to SAU and UAE found that the upsurge in cases in both countries was due to several hospital-acquired outbreaks that resulted from a lack of systematic implementation of infection prevention and control measures.
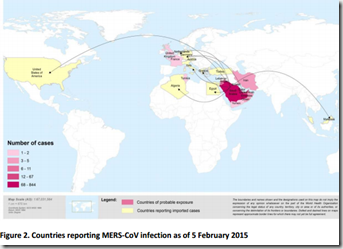
Since mid-May, the numbers of cases in SAU and UAE have sharply declined. However, cases continue to be reported from SAU, some of which reflect nosocomial transmission in hospitals in Taif city, Jubail city, Eastern Region and Riyadh.Although the number of cases reported from SAU has been relatively small, the cases occurred in several regions across SAU, suggesting that zoonotic transmission is allowing the virus to infect humans residing in several locations across the country, and that human-to-human transmission in healthcare settings continues. The risk of exported cases from SAU remains. Since the last update, three cases with exposure in SAU have been reported by Austria, Jordan and Turkey. No onward transmission has been observed in these three countries.
The WHO team concluded that the cluster of MERS-CoV cases in Kerman, Iran, in May and June 2014, showing epidemiological evidence of healthcare-associated transmission, could possibly have been caused by a combination of factors. These included inconsistent application of infection prevention and control measures in a healthcare setting at the beginning of the outbreak, as well as weakness in the surveillance system to actively follow and identify cases.
Surveillance has been enhanced and preparedness activities have been implemented in Kerman province and other parts of the country and there have been no reports of further cases in the affected hospital, in Kerman province, or the rest of the country.
Also in October, two cases were reported by Qatar. One case became ill while travelling from Qatar to SAU and sought medical treatment in Al-Hasa, SAU, and the other case had reported recent contact with camels and camel milk in Qatar. An estimated 1.4 million people travelled to SAU for Hajj in October 2014. Enhanced surveillance during Hajj, upon exit from the country and in the countries of the returning pilgrims did not identify any MERS-CoV cases.
Investigations in SAU and UAE took place in 2013-2014 to evaluate the role of asymptomatic PCRpositive cases in human-to-human transmission. It has been suggested that there may have been human-to-human transmission from asymptomatic cases in the UAE and SAU; however, in these instances, not all other potential sources of transmission have been ruled out. It is also currently not clear whether asymptomatic cases were asymptomatic at the time of reporting and remained asymptomatic, or later developed symptoms, as the follow-up of a number of recently reported asymptomatic cases have documented mild symptoms. Until more is known, and when resources allow, close monitoring and investigation of all contacts, including asymptomatic contacts, should be conducted.
Risk AssessmentHas the transmission pattern of MERS-CoV changed?
Based on available information from recent cases, there is neither evidence of sustained human-to human transmission in the community nor evidence of airborne transmission. Therefore, the overall transmission patterns previously observed remain unchanged. WHO bases this assessment on the evidence that:
- The clinical picture appears to be similar to that observed previously; secondary cases tend to present with milder disease than primary cases, and many of the recently reported secondary cases have been mild, or were people whose tests were positive for MERS-CoV but were asymptomatic;
- The cases recently exported to other countries have not resulted in sustained onward transmission to persons in close contact with these cases on airplanes or in the respective countries outside the Middle East ;
- Intensive screening of MERS-CoV contacts revealed very few instances of household transmission; and
IV. There has been no increase in the size or number of observed household clusters.
Can we expect additional cases of MERS-CoV infection in the Middle East? And can we
expect additional cases exported to other countries?WHO expects that additional cases of MERS-CoV infection will be reported from the Middle East, and it is likely that cases will continue to be exported to other countries by tourists, travellers, migrant workers or pilgrims who might acquire infection after exposure to an animal (for example, while visiting farms or markets) or human source (possibly in a health care setting). Until more is understood about mode of transmission and risk factors for infection, cases resulting from zoonotic transmission will continue to occur, and will eventually lead to limited community transmission within households and possibly significant hospital-associated outbreaks. Among the recently exported cases who reported performing Umrah in SAU, investigation into their activities while in SAU revealed that they had either visited a healthcare facility or had come into contact with camels or raw camel products while in SAU.