|
| Credit CDC PHIL |
#11,311
In the 75 year history of antibiotics, one truth has been apparent from almost the beginning; over time, and particularly with repeated exposure, bacteria can become resistant to antimicrobials.
Even before penicillin could be rolled out for clinical use, a β-lactamase (Penicillinase) was identified by researchers Abraham and Chain in a sample of Gram-negative E. coli in 1940 (cite).
Over the next two decades penicillinase resistance spread to other bacteria, which required the creation of newer generations of the drug (such as Methicillin in 1959), that were resistant to these enzymes.
Methicillin resistance emerged in the UK only 2 years later, and while it is no longer used, we retain its name in the term MRSA (Methicillin-resistant Staphylococcus aureus) (cite).
One of the earliest, and most important uses for penicillin was in curing gonorrhea. But by the 1970s penicillin/tetracycline resistant forms of Neisseria gonorrhoeae began to appear in the United States, and eventually cephalosporins replaced them as the first-line treatment for gonorrhea.
In 1993, the CDC also recommended the use of fluoroquinolones (i.e., ciprofloxacin, ofloxacin, or levofloxacin) to treat gonorrhea, as they were relatively cheap, effective, and allowed for a 1 dose treatment.
But in less than a decade, fluoroquinolone-resistant N. gonorrhoeae (QRNG) emerged out of Asia and began showing up in Hawaii and then California (see MMWR Increases in Fluoroquinolone-Resistant Neisseria gonorrhoeae --- Hawaii and California, 2001).
In 2007, the CDC announced Fluoroquinolones No Longer Recommended for Treatment of Gonococcal Infections, leaving just one class of antibiotics - the cephalosporins - still recommended and available for the treatment of gonorrhea.
Today, a combination therapy of a cephalosporin (cefixime or ceftriaxone), along with a macrolide antibiotic (preferably azithromycin) are the only recommended treatments that remain for Gonorrhea.
But given the above history, it no surprise that we are beginning to see cracks in this last line of defense. A few past blogs include:
Last December following an outbreak of an outbreak of `super gonorrhea' in Leeds, England (cite BBC report), Dame Sally Davies - England's Chief Public Health Officer - issued a dire warning that: Gonorrhoea 'could become untreatable'.
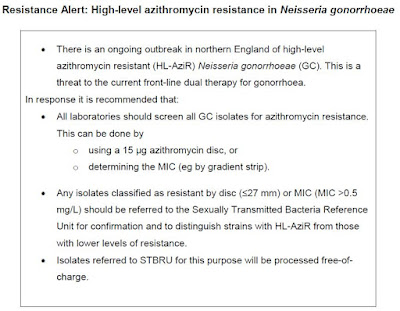
Last October a National Resistance Alert was issued in the UK ordering all gonococcal samples tested for azithromycin resistance and that resistant isolates be referred to PHE’s Sexually Transmitted Bacteria Reference Unit (STBRU).
Fast forward to mid-April, and the UK's PHE published a new report (Outbreak of high level azithromycin resistant gonorrhoea in England) detailing the spread of their `super gonorrhea outbreak' well beyond Leeds (excerpts below).
Volume 10 Number 15 Published on: 15 April 2016
Outbreak of high level azithromycin resistant gonorrhoea in England
There have been 34 cases of high level azithromycin resistant gonorrhoea (HL-AziR) (MIC >256 mg/L) diagnosed amongst residents of England between November 2014 and April 2016 (see figure). HL-AziR has previously been observed only sporadically in the UK and elsewhere.
Cases of highly azithromycin-resistant Neisseria gonorrhoeae 2014 to February2016
The outbreak first emerged in residents of Leeds and the north of England [1]. The outbreak has since spread to the West Midlands and south of England, including London. Initial cases were among heterosexuals but more recent evidence suggests HL-AziR is now spreading among men who have sex with men. Partner notification has been of limited success: of 50 partners thus far reported, only 22 (44%) were successfully contacted, 18 (82%) of which were tested; 17 (94%) tested positive for gonorrhoea. Whole genome sequencing of a subset of the isolates indicates that many of the isolates were clonal, consistent with recent transmission, and the remainder are closely related and share a more distant common ancestor.
(continue . . . )
This continuing geographic expansion of resistant gonorrhea in England has prompted PHE to issue a fresh Resistance alert: high-level azithromycin resistance in Neisseria gonorrhoeae dated May 2016.
If you haven't already seen it, I highly recommend you view: