#14,143
Despite the abrupt slowdown in MERS case reports coming out of Saudi Arabia the past couple of months, with less than half the year gone, KSA has already surpassed 2018's total number of cases (see WHO graphic below).
These are only the identified and officially reported cases, as there is pretty good evidence to suggest that many cases go undiagnosed, or misdiagnosed. This is not, however, a problem limited to Saudi Arabia.
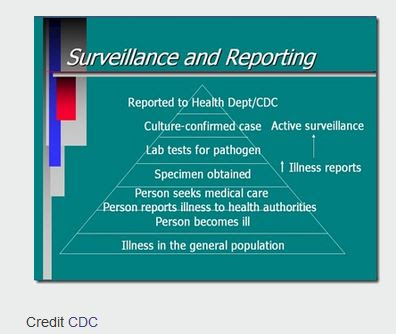
As the CDC graphic below illustrates, almost all surveillance programs pick up the `tip of the pyramid', of disease cases in any community. This holds true whether you are talking about MERS in the Middle East, Avian flu in China, or Lyme Disease or West Nile Fever in the United States.
More specifically for MERS-CoV, however:
- In November of 2013, we looked at a study published in The Lancet Infectious Diseases, that estimated for every case identified, there are likely 5 to 10 that go undetected.
- In 2015, when Saudi Arabia had recorded fewer than 1200 MERS cases, a seroprevalence study (see Presence of Middle East respiratory syndrome coronavirus antibodies in Saudi Arabia: a nationwide, cross-sectional, serological study by Drosten & Memish et al.,) suggested nearly 45,000 might have been infected.
- And a 2016 study (see EID Journal: Estimation of Severe MERS Cases in the Middle East, 2012–2016) suggested that as much as 60% of severe Saudi MERS cases go undiagnosed.
J. Korean Med Sci: Atypical Presentation Of A MERS Case In A Returning Traveler From Kuwait
mBio: High Prevalence of MERS-CoV Infection in Camel Workers in Saudi Arabia
AJIC:Intermittent Positive Testing For MERS-CoV
JIDC: Atypical Presentation Of MERS-CoV In A Lebanese PatientAnd last August - in Evaluation of a Visual Triage for the Screening of MERS-CoV Patients - we also looked at what has been described as a serious flaw in Saudi Arabia's MERS surveillance program.
With those caveats in place, today KSA reports their 2nd primary (both with camel contact) MERS case of Epi Week 25 (see below).
While MERS-CoV hasn't taken off the way that SARS-CoV did 16 years ago, we've seen studies (see A Pandemic Risk Assessment Of MERS-CoV In Saudi Arabia) suggesting the virus doesn't have all that far to evolve before it could pose a genuine global threat.
A little over year ago in the WHO List Of Blueprint Priority Diseases, we saw MERS-CoV listed among the 8 disease threats in need of urgent accelerated research and development.Among the tools needed are faster, and more accurate diagnostic tests, and an effective armamentarium of drugs and/or vaccines. Unless and until they become available, MERS is likely to continue to spark household and nosocomial outbreaks and remain a serious public health concern.