|
| Credit WHO |
#14,528
A couple of weeks ago, in WHO Guidance: Non-pharmaceutical Public Health Measures for Mitigating the Risk and Impact of Epidemic and Pandemic Influenza, we took our first look at the World Health Organization's recently released 91-page NPI Guidance document.
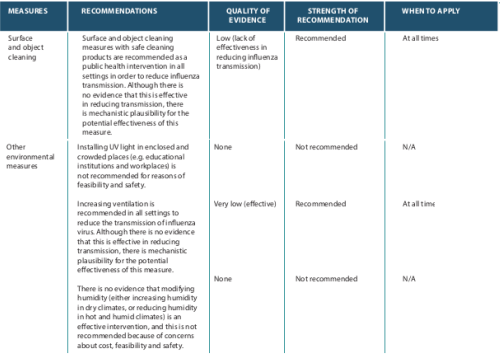
Since then we've taken a closer look at the WHO's recommendations on Personal protective NPIs (hand hygiene, isolation, masks, etc.) and Social Distancing.Today we'll look at the WHO recommendations for Environmental measures that could help reduce the spread, and hopefully the impact, of a pandemic (see Community Pandemic Mitigation's Primary Goal : Flattening The Curve).
These include surface and object cleaning, UV lights, ventilation, and adjusting indoor humidity levels.The WHO bases their recommendations on the best available scientific evidence on their effectiveness - tempered by practical considerations and potential harms - but admits that in many cases the quality of scientific evidence is low, or even absent.
The major points are summarized in the chart below, after which we'll look at them individually.
Surface and Object Cleaning
Although most flu transmission is likely via a respiratory route, studies have found that infectious flu particles can remain viable for hours - or even days - on some surfaces (fomites).
When people touch a contaminated surface, they can not only infect themselves (generally by touching their mouth, nose, or eyes), they can carry the virus to other places and deposit them on new surfaces.Five years ago, in ICAAC Video: How Quickly A Virus Can Spread In A Building, we looked at a study that showed that viruses from a single contaminated surface (door knob, tabletop, etc.) in an office environment can spread to contaminate an entire building in a matter of hours.
More recently, in 2018's Simulated Influenza A Transmission In An Office Environment - researchers found that `. . . long-range airborne, fomite and close contact routes contribute to 54.3%, 4.2% and 44.5% of influenza A infections, respectively.
They also noted that `Keyboards, headphones, desktops, mice and mobile phones are the five most-contaminated private surfaces around the infected student.'Even though a minority of flu infections appear to be due to touching contaminated fomites, cleaning and disinfecting common surfaces ought to have some impact on the rate of transmission, and have little downside.
The WHO recommends surface and object cleaning for all epidemic and pandemic severity levels:
UV Lights
Although conventional UV lights can be quite effective in killing flu viruses, exposure can be both carcinogenic and cataractogenic, which severely limits how they can be used in public.
A couple of years ago party goers at Hong Kong's Landmark experienced skin burns and eye damage when the wrong type of UVC lamps were used at a public event (see Partygoers left with burns and light sensitivity after Hypebeast event at The Landmark).There are UV wavelengths (Far-UVC : 207–222 nm) that are much safer, yet still effective in killing viruses, but the equipment costs remain high (see Far-UVC light: A new tool to control the spread of airborne-mediated microbial diseases).
Given the costs, and the potential for the wrong type of UV lighting equipment to be used, the WHO has decided not to recommend UV lights as an NPI.
 |
Ventilation
During the 1918 pandemic, people were advised to keep their windows open, and trolley cars routinely increased ventilation (and reduced the number of riders) in order to slow the spread of the flu.
 |
| Credit National Archives |
While most of the evidence from 1918 is anecdotal, many believe those practices helped to significantly reduce transmission of the virus. The WHO cites a couple of modern studies (see below) in making a positive recommendation.
Increased ventilation
Summary of evidence
A simulation study predicted a reduction of transmission among kindergarten students by enhancing the air changes per hour (ACH) (92). Two simulation studies evaluated the effectiveness of increasing ventilation in reducing influenza transmission in community settings (93, 94). One of these two studies suggested a reduction of daily peak infections by increasing ACH under the baseline scenario (93), and the other predicted that the peak infection rate could be reduced by more than 60% by doubling or tripling the ventilation rate (94).
The rub here being that in most modern commercial buildings (built in the last 50 years), windows don't open, and air exchange is handled by the building's HVAC system. In most homes, open windows are an option, but only when temperatures aren't uncomfortably high or low.
Modifying Humidity
Over the past decade we've looked at a number of studies indicating that influenza viruses survive longer in the environment when temperature and humidity fall within certain ranges.
- In 2008 researchers Jeffrey Shaman and Melvin Kohn established a correlation between the AH (Absolute Humidity) and the survival, and transmission of the influenza virus (see It's Not So Much The Heat, It's The Humidity).
-
A 2012 study (see Influenza Virus Survival At Opposite Ends Of The Humidity Spectrum) found both extremely low and extremely high humidity
were conducive to flu transmission – at least when it resides in mucus
and respiratory fluids like those found in your nose, throat, or lungs.
- In 2013, in NIH Study: Climate & Influenza Transmission, we looked at a PLoS One study called High Humidity Leads to Loss of Infectious Influenza Virus from Simulated Coughs that concluded that `. . . maintaining indoor relative humidity at levels greater than 40% can significantly reduce the infectious capacity of aerosolized flu virus.'
- In 2018's bioRxIv: Humidity As A Non-pharmaceutical Intervention For Influenza A, researchers reported finding: An increase in average AH from 6.33 mb in control rooms to 9.89 mb in humidified rooms (RH ~42-45 %) was associated with a significant decrease in influenza A virus presence in fomite and air samples in humidified rooms compared to control rooms.
In 2011 we followed an outbreak of Idiopathic pulmonary fibrosis (IPF) that was ultimately traced to the sterilizing fluid used in home humidifiers, while humidifiers have also been linked to increased asthma in children and to rare legionella infection.While better data may come out of the next pandemic, for now, the WHO is not recommending modifying humidity as an NPI during the next influenza pandemic.
Taken individually, none of these recommended NPIs are likely to do very much. But when `layered' on top of one another, they can reduce the number of people infected at any given time.
While it probably won't make much of a difference in the number of illnesses or deaths caused by the virus, by spreading them out over a longer time period you can hopefully reduce the amount of collateral damage to society.
We'll finish out this series by looking at the WHO travel related NPIs in a future blog.