#15,221
Due to the uncertain arrival date and subsequent spread of COVID-19 into the United States, a precise split between the impact of this year's flu season and the novel coronavirus may take years to unravel.
Surveillance for COVID-19 prior to March 1st was spotty at best, and many `influenza' cases - and deaths - early in 2020 may have been due to the pandemic virus.And that may explain the unusually wide range provided by this year's CDC Influenza Burden Estimates (see above), which range from 24,000 to 62,000 deaths. The low end (24,000) would represent a relatively mild-to-moderate flu season, while the top end (62,000) would suggest a severe-to-high severe season.
But what we do know is, since the United States began its `15 days to Stop the Spread' of COVID-19 in Mid-March, the rate of ILI visits and hospitalizations began to fall dramatically (see FluView chart below).
The mitigation efforts against COVID-19 appear to have had a similar impact on reducing the spread and burden of influenza. While the rate of influenza might have fallen off a cliff by early April on its own accord, we've similar reports today - published in the CDC's EID Journal - of flu suppression starting even earlier in nations that began COVID-19 mitigation in January.
First links and brief excerpts from these reports, then I'll return with a postscript.
Volume 26, Number 8—August 2020
Research Letter
Decreased Influenza Incidence under COVID-19 Control Measures, Singapore
Roy Jiunn Jye Soo, Calvin J. Chiew, Stefan Ma, Rachael Pung, and Vernon Lee
Abstract
We compared indicators of influenza activity in 2020 before and after public health measures were taken to reduce coronavirus disease (COVID-19) with the corresponding indicators from 3 preceding years. Influenza activity declined substantially, suggesting that the measures taken for COVID-19 were effective in reducing spread of other viral respiratory diseases.(SNIP)
Our study has several limitations. First, a decrease in influenza transmission is expected in February–March, given the yearly bimodal pattern of influenza incidence in Singapore (5). However, the decrease in 2020 is marked compared to previous years. Second, there could be fewer ILI visits to government clinics because of altered health-seeking behavior, or cases may be referred to hospitals and therefore not captured as ILI cases in clinics. However, these missed ILI cases would not affect the proportion positive for influenza. Third, we can infer similar effects on COVID-19 only if the transmission dynamics are similar to influenza.
In conclusion, we found a marked decline in ILI in Singapore after the implementation of public health measures for COVID-19. Our findings suggest that such measures are effective in reducing spread of viral respiratory diseases and could mitigate the impact of the COVID-19 pandemic.(Continue . . . )
Volume 26, Number 8—August 2020
Research Letter
Collateral Benefit of COVID-19 Control Measures on Influenza Activity, TaiwanShu-Chen Kuo, Shu-Man Shih, Li-Hsin Chien, and Chao A. Hsiung
Abstract
Taiwan has strictly followed infection control measures to prevent spread of coronavirus disease. Meanwhile, nationwide surveillance data revealed drastic decreases in influenza diagnoses in outpatient departments, positivity rates of clinical specimens, and confirmed severe cases during the first 12 weeks of 2020 compared with the same period of 2019.
(SNIP)
The functional healthcare and surveillance systems in Taiwan, the government’s efforts to identify causes of ILI during the COVID-19 pandemic, and sufficient laboratory capacity ensure appropriate influenza testing and reporting of results. Healthcare avoidance during COVID-19 pandemic may be an important confounder for the results we reported. However, because of awareness of the similarities in symptoms between COVID-19 and influenza and the low number of COVID-19 patients in Taiwan ( < 200 cases as of March 21, 2020), patients with ILI would not avoid seeking medical help for a diagnosis. Healthcare avoidance also did not explain the lower number of severe influenza cases observed in 2020 (Figure, panel D).
Therefore, we believe that the decreasing influenza activity in Taiwan in 2020 is the result of strict control measures that were established in response to COVID-19.
(Continue . . . )
These findings, much like the drop in car accidents and other trauma during our national lockdown, are not unexpected.
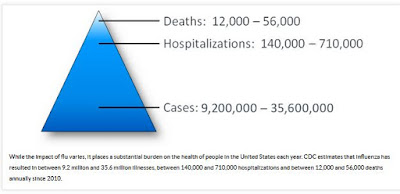
During particularly severe flu seasons, the United States can see between 60,000 and 80,000 deaths due to influenza. But even during a `normal' flu season, between 12,000 and 56,000 Americans can die, and that can include several hundred kids (under 18).
 |
| https://www.cdc.gov/flu/about/disease/burden.htm |
While shutting down society and crippling the economy every flu season is out of the question, there are a number of low impact things we can do - such as wearing face covers or masks in public, using hand sanitizer, and staying home if you are sick - that just might shave a few thousand deaths off influenza's yearly butcher's bill.
We've already evidence the concept works, and proof that the American public - once rallied - can adapt to new mitigation efforts. And next winter will likely only reinforce those habits.
While it has been cynically said that one should never let a perfectly good crisis go to waste, I prefer to think of this as a teachable moment.If we come out of this pandemic with a new found respect for seasonal flu - and a broad commitment towards practicing better flu hygiene as a society every winter - then the lessons of COVID-19 could continue to save lives for years to come.
And it just might give us an edge the next time a novel respiratory virus decides to call in the middle of flu season.

