How to Wear Face Cover -CDC
#15,300
Given that NPIs - or Nonpharmaceutical Interventions - have long been considered key to slowing a pandemic (see 2007's The CDC Does NPI), it has been remarkable how long it has taken many public health entities to accept and/or endorse the value of one of the most basic - and sensible - NPI measures; the wearing of face covers by the public.
Although their use is nearly universal in Asia during regular flu season and during this pandemic, in the west their use was initially either ridiculed as ineffective or heavily discouraged (see WHO Interim Advice On The Community, Home, Healthcare Use of Masks For nCoV2019s and the infamous Feb 29th tweet by the U.S. Surgeon General).
This, despite several past studies suggesting that face masks and coverings are likely reasonably effective in reducing respiratory illness. In 2014's Efficacy Of Hand Hygiene Alone Against Influenza Infection, we looked at Dr. Allison Aiello's multi-year study at the University of Michigan that compared the effectiveness of handwashing and facemasks (alone, and in combination) at reducing the spread of seasonal influenza in a college dorm setting.
Their results?
Neither face mask use and hand hygiene nor face mask use alone was associated with a significant reduction in the rate of ILI, although combined, they produced a 35% to 51% reduction of infection over the control group.Another study, this time in PLoS One found:
Professional and Home-Made Face Masks Reduce Exposure to Respiratory Infections among the General PopulationAnd for further proof, we only need look at the disparity in COVID-19 cases (and deaths) between western nations which were generally late to adopt face covers, and Asian nations - like Taiwan and South Korea - which heavily promoted (or even required) their use by the public from the beginning.
Marianne van der Sande , Peter Teunis, Rob Sabel
Taiwan, which was one of the first countries outside of China to beaffected by COVID-19, today has reported a total of 428 cases, and just 8 deaths.
Despite this evidence of benefit, I'm seeing growing mask `fatigue' - at least here in central Florida - as more and more people go to the store, or work, without face covers. I get it, it's hot and muggy here, and masks can quickly become uncomfortable.
Bu today we've two new studies - one in the Lancet and the other in the EID Journal - that suggest that controlling COVID-19's spread without using the full range of NPIs will be both longer and more difficult.
Next stop, The Lancet, where a new systematic review and meta-analysis is even more on point, although some of the evidence of efficacy is limited and none of these precautions - whether combined or individually - can provide complete protection against infection.
Bu today we've two new studies - one in the Lancet and the other in the EID Journal - that suggest that controlling COVID-19's spread without using the full range of NPIs will be both longer and more difficult.
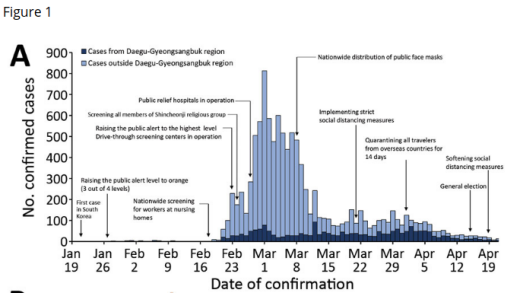
First stop, the CDC's EID Journal, which has a dispatch on how South Korea's use of NPIs - and without resorting to a full lockdown - how that enabled them to quickly curtail a massive outbreak of COVID-19.While South Korea has reported a recent surge in cases (49 reported in the past 24 hours), their overall numbers remain enviable (n=11,590 cases and 273 deaths).
Admittedly, face masks were just one part of their NPI strategy, but you'll note in Figure 1 that the first dramatic reduction in cases came about a week after the nationwide distribution of public face masks.Follow the link to read the study in its entirety.
Volume 26, Number 10—October 2020
Dispatch
Effect of Nonpharmaceutical Interventions on Transmission of Severe Acute Respiratory Syndrome Coronavirus 2, South Korea, 2020
Sukhyun Ryu, Seikh Taslim Ali, Cheolsun Jang, Baekjin Kim, and Benjamin J. Cowling
Author affiliations: Konyang University College of Medicine, Daejeon, South Korea (S. Ryu, C. Jang, B. Kim); The University of Hong Kong, Hong Kong, China (S.T. Ali, B.J. Cowling)
Abstract
We analyzed transmission of coronavirus disease outside of the Daegu-Gyeongsangbuk provincial region in South Korea. We estimated that nonpharmaceutical measures reduced transmissibility by a maximum of 34% without resorting to a strict lockdown strategy. To optimize epidemic control, continuous efforts to monitor the transmissibility are needed.
(SNIP)
Our findings suggest that the nonpharmaceutical interventions implemented in South Korea during the COVID-19 outbreak effectively reduced virus transmissibility and suppressed local spread. However, the population of South Korea is still susceptible to further outbreaks or epidemic waves. Because social distancing measures will be relaxed while opportunities for importation of infections from abroad continue, ongoing monitoring of the effective reproductive number can provide relevant information to help policymakers control a potential second wave of COVID-19.
(Continue . . . )
Next stop, The Lancet, where a new systematic review and meta-analysis is even more on point, although some of the evidence of efficacy is limited and none of these precautions - whether combined or individually - can provide complete protection against infection.
Follow the link to read the study in its entirety. You'll find excerpts from a press release, and a graphic follow.
Whether it is due to pride, hubris, or a misplaced fear of alarming the public or hurting the economy, we seem to have a habit not pulling the trigger early when faced with a public health crisis.
Something as simple as recommending the wearing of face covers (see The Man In The Ironed Mask) and social distancing for the public last January might have reduced the spread of COVID-19 in the United States, and avoided or shortened our 6 week lockdown.
Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis
Derek K Chu, MD, Prof Elie A Akl, MD, Stephanie Duda, MSc, Karla Solo, MSc, Sally Yaacoub, MPH, Prof Holger J Schünemann, MD et al.
Open Access Published:June 01, 2020
DOI:https://doi.org/10.1016/S0140-6736(20)31142-9
Findings
Our search identified 172 observational studies across 16 countries and six continents, with no randomised controlled trials and 44 relevant comparative studies in health-care and non-health-care settings (n=25 697 patients).
Transmission of viruses was lower with physical distancing of 1 m or more, compared with a distance of less than 1 m (n=10 736, pooled adjusted odds ratio [aOR] 0·18, 95% CI 0·09 to 0·38; risk difference [RD] −10·2%, 95% CI −11·5 to −7·5; moderate certainty); protection was increased as distance was lengthened (change in relative risk [RR] 2·02 per m; pinteraction=0·041; moderate certainty).
Face mask use could result in a large reduction in risk of infection (n=2647; aOR 0·15, 95% CI 0·07 to 0·34, RD −14·3%, −15·9 to −10·7; low certainty), with stronger associations with N95 or similar respirators compared with disposable surgical masks or similar (eg, reusable 12–16-layer cotton masks; pinteraction=0·090; posterior probability >95%, low certainty). Eye protection also was associated with less infection (n=3713; aOR 0·22, 95% CI 0·12 to 0·39, RD −10·6%, 95% CI −12·5 to −7·7; low certainty). Unadjusted studies and subgroup and sensitivity analyses showed similar findings.
Interpretation
The findings of this systematic review and meta-analysis support physical distancing of 1 m or more and provide quantitative estimates for models and contact tracing to inform policy. Optimum use of face masks, respirators, and eye protection in public and health-care settings should be informed by these findings and contextual factors. Robust randomised trials are needed to better inform the evidence for these interventions, but this systematic appraisal of currently best available evidence might inform interim guidance.
(Continue . . . )From the Press Release:
- First review of all available evidence including 172 observational studies looking at how physical distancing, face masks, and eye protection affect the spread of COVID-19, SARS, and MERS in both community and healthcare settings across 16 countries.
- Physical distancing of at least 1 metre lowers risk of COVID-19 transmission, but distances of 2 metres could be more effective.
- Face coverings and masks might protect both healthcare workers and the general public against infection with COVID-19, and protective eye covering may also provide additional benefit--although the certainty of the evidence is low for both forms of protection.
- Importantly, even when properly used and combined, none of these interventions offers complete protection and other basic protective measures (such as hand hygiene) are essential to reduce transmission.
Whether it is due to pride, hubris, or a misplaced fear of alarming the public or hurting the economy, we seem to have a habit not pulling the trigger early when faced with a public health crisis.
Something as simple as recommending the wearing of face covers (see The Man In The Ironed Mask) and social distancing for the public last January might have reduced the spread of COVID-19 in the United States, and avoided or shortened our 6 week lockdown.
Unfortunately, it didn't happen, so we'll never know.In some ways we've been lucky with COVID-19. As bad as it has been, it hasn't proven to be a high-mortality pandemic like we might expect with MERS-CoV or H5 or H7 avian influenza, and we actually had a few weeks of early warning.
The next time, we may not be as lucky, and similar delays of days or weeks in pulling the trigger could prove far more disastrous. Hopefully we'll be smart enough to learn from our past mistakes.If not, I'm sure nature will find new ways to drum that lesson into our heads until we do.