COVID Epi Curve - Credit WHO
#16,263
Although COVID first came to light during the winter months of 2019-2020, and reached its first peak almost a year later (Dec 2021), its intensity plunged in January of this year, only to reach new heights in the spring. After another lull, the summer of 2021 saw a rise nearly equal to last winter (see epi chart above).
Four years ago, in PLoS Comp. Bio.: Spring & Early Summer Most Likely Time For A Pandemic, we looked at evidence that most flu pandemics have emerged when influenza prevalence is low, even though they just about always become seasonal viruses themselves.Pandemic viruses - particularly during their first year or two, when community immunity to a novel virus is low or non-existent - can pose an all-season threat.
Yesterday researchers from Barcelona's Institute for Global Health published a paper in Nature Computational Science that finds `robust' statistical evidence for COVID being a seasonal virus, and provides further evidence of its `airborne' nature.While I think there's been a general expectation that COVID would become a seasonal virus - much like influenza - one that is most prevalent during colder/dryer winter seasons, its behavior until now has raised questions.
All of which has implications - not only for this winter - but potentially for winters to come.
I've reproduced (translated) excerpts from their press release, and a link and the abstract to the study, but you'll want to follow the link to read the research in its entirety. I'll have a brief postscript after the break.
(Translated)
RESEARCH
New Study Provides Robust Evidence that COVID-19 is a Seasonal Infection
By using a statistical method designed to detect transitory associations as well as a mathematical model, the authors show that climate played a strong role in modulating viral transmission during the pandemic waves in both hemispheres21.10.2021
A new study led by ISGlobal, an institution supported by “la Caixa” Foundation, provides robust evidence that COVID-19 is a seasonal infection linked to low temperatures and humidity, much like seasonal influenza. The results, published in Nature Computational Science, also support the considerable contribution of airborne SARS-CoV-2 transmission and the need to shift to measures that promote “air hygiene”.
A key question regarding SARS-CoV-2 is whether it is behaving, or will behave, as a seasonal virus like influenza, or whether it will be equally transmitted during any time of the year. A first theoretical modelling study suggested that climate was not a driver in COVID-19 transmission, given the high number of susceptible individuals with no immunity to the virus. However, some observations suggested that the initial propagation of COVID-19 in China occurred in a latitude between 30 and 50o N, with low humidity levels and low temperatures (between 5o and 11o C).
“The question of whether COVID-19 is a genuine seasonal disease becomes increasingly central, with implications for determining effective intervention measures,” explains Xavier Rodó, director of the Climate and Health programme at ISGlobal and coordinator of the study. To answer this question, Rodó and his team first analysed the association of temperature and humidity in the initial phase of SARS-CoV-2 spread in 162 countries across five continents, before changes in human behaviour and public health policies were put into place. The results show a negative relationship between the transmission rate (R0) and both temperature and humidity at the global scale: higher transmission rates were associated with lower temperatures and humidity.
The team then analysed how this association between climate and disease evolved over time, and whether it was consistent at different geographical scales. For this, they used a statistical method that was specifically developed to identify similar patterns of variation (i.e. a pattern-recognition tool) at different windows of time. Again, they found a strong negative association for short time windows between disease (number of cases) and climate (temperature and humidity), with consistent patterns during the first, second and third waves of the pandemic at different spatial scales : worldwide, countries, down to individual regions within highly affected countries (Lombardy, Thüringen and Catalonia) and even to the city level (Barcelona).
The first epidemic waves waned as temperature and humidity rose, and the second wave rose as temperatures and humidity fell. However, this pattern was broken during summertime in all continents. “This could be explained by several factors, including mass gatherings of young people, tourism, and air conditioning, among others,” explains Alejandro Fontal, researcher at ISGlobal and first author of the study.
When adapting the model to analyse transient correlations at all scales in countries in the Southern Hemisphere, where the virus arrived later, the same negative correlation was observed. The climate effects were most evident at temperatures between 12o and 18oC and humidity levels between 4 and 12 g/m3, although the authors warn that these ranges are still indicative, given the short records available.
Finally, using an epidemiological model, the research team showed that incorporating temperature into the transmission rate works better for predicting the rise and fall of the different waves, particularly the first and third ones in Europe. “Altogether, our findings support the view of COVID-19 as a true seasonal low-temperature infection, similar to influenza and to the more benign circulating coronaviruses,” says Rodó.
This seasonality could contribute importantly to the transmission of SARS-CoV-2, since low humidity conditions have been shown to reduce the size of aerosols, and thereby increase airborne transmission of seasonal viruses such as influenza. “This link warrants an emphasis on ‘air hygiene’ through improved indoor ventilation as aerosols are capable to persist suspended for longer times,” says Rodó, and highlights the need to include meteorological parameters in the evaluation and planning of control measures.
Published: 21 October 2021
Climatic signatures in the different COVID-19 pandemic waves across both hemispheres
Alejandro Fontal, Menno J. Bouma, Adrià San-José, Leonardo López, Mercedes Pascual & Xavier RodóAbstract
The roles of climate and true seasonal signatures in the epidemiology of emergent pathogens, and that of SARS-CoV-2 in particular, remain poorly understood. With a statistical method designed to detect transitory associations, we show, for COVID-19 cases, strong consistent negative effects of both temperature and absolute humidity at large spatial scales.At finer spatial resolutions, we substantiate these connections during the seasonal rise and fall of COVID-19. Strong disease responses are identified in the first two waves, suggesting clear ranges for temperature and absolute humidity that are similar to those formerly described for seasonal influenza. For COVID-19, in all studied regions and pandemic waves, a process-based model that incorporates a temperature-dependent transmission rate outperforms baseline formulations with no driver or a sinusoidal seasonality.Our results, so far, classify COVID-19 as a seasonal low-temperature infection and suggest an important contribution of the airborne pathway in the transmission of SARS-CoV-2, with implications for the control measures we discuss.
While the current decline in COVID around the world has been a welcomed development - it appears to have leveled off in recent weeks - and that, combined with these findings, should give us pause over what we might see later this winter or perhaps in the spring.
The 1957 H2N2 pandemic famously pulled a disappearing act over the summer and winter of 1958 and for most of 1959, only to abruptly return late in the year - and again four years later in 1963.
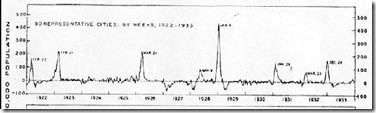
H2N2 Pandemic Waves - NEJM 2009
While the 1918 H1N1 pandemic was officially declared `over' in 2019, the United States - and the rest of the world - saw frequent flareups of influenza over the the decade that followed. In 1922, 1923, 1925, and 1928 spikes were well above the baseline (see 2008's Sometimes . . . Out Of The Blue).
How COVID will react this winter, and in winters that follow, will depend not only on the virus and its evolution, along with climatic conditions, but on the durability of our community immunity. Whether naturally acquired, or vaccine induced, immunity will likely wane over time.
Which suggests - even if we get lucky, and COVID doesn't present another big wave this winter - the threat won't necessarily have gone away.
It could just be biding its time, until the conditions are ripe for a return.