https://www.medrxiv.org/content/10.1101/2022.02.27.22271328v1.full.pdf
While not unique to SARS-COV-2 infection, with literally hundreds of millions of COVID survivors, even a small percentage of Long COVID patients would yield millions of cases.
The CDC describes it this way:
Overview
Although most people with COVID-19 get better within weeks of illness, some people experience post-COVID conditions. Post-COVID conditions are a wide range of new, returning, or ongoing health problems people can experience four or more weeks after first being infected with the virus that causes COVID-19. Even people who did not have COVID-19 symptoms in the days or weeks after they were infected can have post-COVID conditions. These conditions can present as different types and combinations of health problems for different lengths of time.
These post-COVID conditions may also be known as long COVID, long-haul COVID, post-acute COVID-19, long-term effects of COVID, or chronic COVID. CDC and experts around the world are working to learn more about short- and long-term health effects associated with COVID-19, who gets them, and why.
Last September the CDC's MMWR carried a report (see Post-Acute Sequelae of SARS-CoV-2 Infection Among Adults Aged ≥18 Years — Long Beach, California, April 1–December 10, 2020) that found:
In a random sample of recovered COVID-19 patients in Long Beach, California, one third of participants reported post-acute sequelae 2 months after their positive test result, with higher rates reported among persons aged ≥40 years, females, persons with preexisting conditions, and Black persons.
This is a topic we've covered often over the past couple of years, including:
Nature: Long-term Cardiovascular Outcomes of COVID-19
CMAJ: Even Mild COVID-19 May Have Long-term Brain Impacts
CDC Science Update: COVID-19 and Persistent Symptoms
JACC: Postacute Sequelae of SARS-CoV-2 Infection: A State-of-The Art Review
Most of the (still limited) information we have on post-COVID syndrome comes from people who were infected with variants that emerged before Omicron, and so it isn't certain how much of an impact this latest, and largest, wave of the pandemic will have on Long COVID numbers.
But today we have the results of the Danish AFTER-COVID survey, which reinforces much of what we already knew, or suspected, about Long COVID, and adds significant detail.
First the summary from Denmark's SSI (Statens Serum Institut) followed by a link and some excerpts from the preprint.
Many Danes experience late effects after covid-19
Researchers at the Statens Serum Institut are now ready with the first results from the world's largest questionnaire survey of late sequelae - AFTER-COVID.
Last edited March 3, 2022
In August 2021, the Statens Serum Institut (SSI) launched the world's largest questionnaire survey of late sequelae associated with covid-19 - AFTER-COVID.
To date, 2 million Danes have been invited to participate, and more than 600,000 have said yes. AFTER-COVID consists of several sub-studies, which include both people who have been infected early in the epidemic and people who are continuously infected.
Now, researchers at SSI are ready to unveil some of the first results from the part of the study that deals with people who were infected early in the epidemic before the delta and omicron variants dominated. And before the vaccination program was widely rolled out. They have answered questionnaires about their physical symptoms 6-12 months after they had been infected.
Large and broad study of 152,880 Danes
In order to take into account the general state of health of the population, the researchers also invited people who had not been infected and asked about their symptoms in everyday life. This made it possible to compare the two groups and get an accurate picture of which symptoms had late effects.
A total of 152,880 Danes participated in this part of EFTER-COVID. Of these, 61,002 were previously infected, and 91,878 had not been infected.
Largest and most representative study
The researchers also asked for information about lifestyle factors. In the same way, they obtained information from the nationwide Danish health registries about chronic diseases and other factors that one can imagine also play a role in the development of late effects.
“Our study is not just the largest questionnaire survey of late effects to date. It is probably also the study that is most representative of a broad population. The comprehensive Danish test strategy has given us some completely unique opportunities to invite participants based on whether they have tested positive or not. This gives us a clear advantage over late-stage studies, which may have only included people who have had a severe covid-19 course ”. says Anna Irene Vedel Sørensen, who is one of the researchers behind the study.
Physical symptoms were common in previously infected
The results were clear. Almost 30% of participants still experienced at least one physical symptom 6-12 months after previous infection.
In participants who had not been infected, it was only 13%.
As the researchers dived further into the numbers, they found that taste and odor disorders along with pronounced fatigue were the most frequent late effects that people experienced. And sickness absence was also higher among the previously infected.
Women are most vulnerable
The large data material also gave the researchers the opportunity to look at who was most exposed to being exposed to late effects.
Here it was clearly women who more often experienced late effects. There was also a predominance of late sequelae in middle-aged people, and in people who had been hospitalized with covid-19.
More on the way from AFTER-COVID about omikron
“It is important to emphasize that the study is based on data from before the delta and omicron variants became dominant, and before the vaccination roll-out took place. We do not expect the milder infection we see today to necessarily manifest itself in the same degree of late effects. But this is something we are working on investigating. Nor can we deny that people with late effects have to a greater extent participated in the study, ”says Professor Anders Hviid from SSI. Together with Professor Steen Ethelberg also from SSI, he leads the AFTER-COVID study.
He continues:
“But there is clearly a picture that the epidemic has affected the health of many Danes for a long time after the acute infection is over. Some might say that the late effects our participants report are not necessarily serious. But it is quite clear that many Danes are experiencing a deterioration in their health. We have to deal with that. ”
The link and abstract follow, although many will want to read the 20-page PDF in its entirety.
Post-acute symptoms, new onset diagnoses and health problems 6 to 12 months after SARS-CoV-2 infection: a nationwide questionnaire study in the adult Danish populationAnna Irene Vedel Sørensen, Lampros Spiliopoulos, Peter Bager, Nete Munk Nielsen, Jørgen Vinsløv Hansen, Anders Koch, Inger Kristine Meder, Steen Ethelberg, Anders Hviiddoi: https://doi.org/10.1101/2022.02.27.22271328
Abstract
Background
A considerable number of individuals infected with SARS-CoV-2 continue to experience symptoms after the acute phase. More information on duration and prevalence of these symptoms in non-hospitalized populations is needed.
Methods
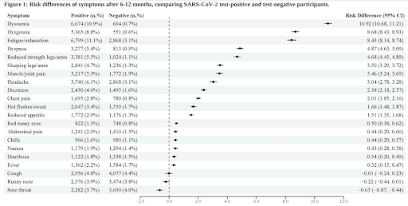
We conducted a nationwide cross-sectional study including 152 880 individuals aged 15-years or older, consisting of RT-PCR confirmed SARS-CoV-2 cases between September 2020-April 2021 (N=61 002) and a corresponding test-negative control group (N=91 878). Data were collected 6, 9 or 12 months after the test using web-based questionnaires. The questionnaire covered acute and post-acute symptoms, selected diagnoses, sick leave and general health, together with demographics and life style at baseline. Risk differences (RDs) between test-positives and -negatives were reported, adjusted for age, sex, single comorbidities, Charlson comorbidity score, obesity and healthcare-occupation.
Findings
Six to twelve months after the test date, the risks of 18 out of 21 physical symptoms were elevated among test-positives and one third (29.6%) of the test-positives experienced at least one physical post-acute symptom. The largest risk differences were observed for dysosmia (RD = 10.92%, 95%CI 10.68-11.21%), dysgeusia (RD=8.68%, 95%CI 8.43-8.93%), fatigue/exhaustion (RD=8.43%, 95%CI 8.14-8.74%), dyspnea (RD=4.87%, 95%CI 4.65-5.09%) and reduced strength in arms/legs (RD=4.68%, 95%CI 4.45-4.89%). More than half (53.1%) of test-positives reported at least one of the following conditions: concentration difficulties (RD=28.34%, 95%CI 27.34-28.78%), memory issues (RD=27.25%, 95%CI 26.80-27.71%), sleep problems (RD=17.27%, 95%CI 16.81-17.73%), mental (RD=32.58%, 95%CI 32.11-33.09%) or physical exhaustion (RD=40.45%, 95%CI 33.99-40.97%), compared to 11.5% of test-negatives. New diagnoses of anxiety (RD=1.15%, 95%CI 0.95-1.34%) or depression (RD=1.00%, 95%CI 0.81-1.19%) were also more common among test-positives.
Interpretation
At the population-level, where the majority of test-positives (96.0%) were not hospitalized during acute infection, a considerable proportion experience post-acute symptoms and sequelae 6-12 months after infection.