#16,699
Omicron variants BA.1.1 and BA.2 have earned the reputation for being `milder' than Delta (and other ancestral strains) of COVID in most of the countries where it has become dominant.While case numbers have soared and people have died, hospitalizations and deaths have not kept pace with increased number of infections.
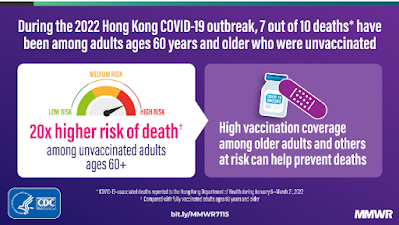
A notable exception being Hong Kong, which had succeeded in keeping the virus from spreading widely in their community for the first two years of the pandemic, and where vaccine uptake - particularly among the elderly - has been tepid.
Hong Kong's high CFR (Case Fatality Rate) - and the spread of BA.2 into the Mainland - is a growing concern for Chinese officials, since the Sinovac vaccines used there are expected to offer little protection against Omicron.
Yonatan Mefsin, Dongxuan Chen, Helen S. Bond, Yun Lin, Justin K. Cheung, Jessica Y. Wong, Sheikh Taslim Ali, Eric H. Y. Lau, Peng Wu, Gabriel M. Leung, Benjamin J. Cowlingdoi: https://doi.org/10.1101/2022.04.07.22273595
ABSTRACT
Hong Kong reported 12,631 confirmed COVID-19 cases and 213 deaths in the first two years of the pandemic but experienced a major wave predominantly of Omicron BA.2.2 in early 2022 with over 1.1 million reported SARS-CoV-2 infections and more than 7900 deaths. Our data indicated a shorter incubation period, serial interval, and generation time of infections with Omicron than other SARS-CoV-2 variants. Omicron BA.2.2 cases without a complete primary vaccination series appeared to face a similar fatality risk to those infected in earlier waves with the ancestral strain.
Several variants of concern of SARS-CoV-2 have caused large outbreaks of infection and substantial mortality following the emergence of the ancestral strain in early 2020. The Omicron variant is the most recent variant to have spread globally, since the first detections in Botswana and South Africa in November 2021 [1, 2]. Hong Kong sustained four small epidemic waves in 2020-2021 with 12,631 confirmed cases cumulatively (1.6 cases per 1000 population). Two vaccines became available in early 2021 including the mRNA vaccine BNT162b2 (BioNTech/Fosun Pharma/Pfizer) and the inactivated vaccine CoronaVac (Sinovac), with 70% of the population receiving two doses of vaccination by 31 December 2021. Community outbreaks of Delta and Omicron viruses began around the end of 2021, with Omicron BA.2.2 ultimately dominating a very large fifth wave which peaked in early March 2022. We characterized the epidemiological features of SARS-CoV-2 infections in the fifth wave in Hong Kong.
Discussion
The SARS-CoV-2 Omicron BA.2 variant has caused more than 1.1 million confirmed cases in Hong Kong (mid-year population 7.4 million) within three months in early 2022, 100-fold higher than all the cases confirmed over four epidemic waves in the previous two years. Not every infection would become a laboratory-confirmed case for various reasons [12]. The peak in the epidemic in early March despite no major change in social distancing measures is likely indicative of a sufficient number of infections to create herd immunity, at least temporarily, with subsequent infections “overshooting” that threshold [13]. Despite stringent public health and social measures, Omicron BA.2.2 spread rapidly with a doubling time of 3.4 days (Figure 1C), quickly outpacing the capacity in test-and-trace, isolation, and quarantine, leading to a large number of patients in need of admission with limited availability of resources. The relatively shorter serial interval and generation time of the Omicron BA.2 subvariant in Hong Kong (Supplementary Figure 3, Supplementary Table 1) compared to earlier variants [14] would have been one of the factors contributing to faster spread in the population along with the higher intrinsic transmissibility (e.g. higher reproductive number).
The high number of deaths in Hong Kong’s fifth wave can be attributed to the high incidence of infections within a short period of time, and the low level of vaccination coverage in older adults. While the overall vaccine coverage at the start of the fifth wave was 70%, in persons ≥65 years and ≥80 years only 50% and 20% had completed a primary series of vaccination. Vaccine hesitancy in older adults occurred for a variety of reasons [15]. Among all the deaths with age recorded up to 23 March, 92.5% (5844/6318) occurred in persons ≥65 years of age and 70.8% (4472/6318) in persons ≥80 years. Infections with the Omicron variant demonstrated attenuated pathogenesis in animal models [16] and milder severity in South Africa [17, 18] and elsewhere [19–21].
However, we found a similar fatality risk for unvaccinated cases in the early part of our fifth wave compared to earlier waves, indicating that the intrinsic severity of BA.2 may not be much lower than the ancestral strain if at all.
We found that cases in persons who had a complete primary series at age of 65-79 years or ≥80 years would have a much lower fatality risk (Figure 2, Supplementary Table 2). In a separate study, we estimated very high vaccine effectiveness against severe disease in older adults ≥60 years of age who received either three doses of the inactivated vaccine CoronaVac or two doses of BNT162b2 [22]. For adults ≥60 years of age, the World Health Organization recommend that three doses of inactivated vaccine are needed [23]. Our estimates of the CFR might slightly overestimate the fatality risk of Omicron in Hong Kong given there was a lack of information on the type of virus variant for all individual cases and a small number of cases including deaths from clusters of Delta infections might have been included in the analysis.
Conclusions
A higher transmission potential was indicated for Omicron variants particularly the BA.2 subvariant in Hong Kong. Cases with a complete primary vaccination series had a much lower fatality risk compared with those without vaccination or with an incomplete primary series of vaccination. Our findings highlighted the importance of achieving a high coverage of vaccination especially in older adults and the need to reassess public health and social measures in control of epidemics in response to a more transmissible SARS-CoV-2 variant in the future.
This is not the first report to have linked the low vaccination rate among those > 60 in Hong Kong to their recent high mortality rate from Omicron BA.2.
Earlier this week we looked at an MMWR report (COVID-19 Mortality and Vaccine Coverage — Hong Kong Special Administrative Region, China, January 6, 2022–March 21, 2022) that came to a similar conclusion.
What is added by this report?
Among persons aged ≥60 years in Hong Kong, 49% had received ≥2 doses of a COVID-19 vaccine, and vaccination coverage declined with age. During January–March 2022, reported COVID-19–associated deaths rose rapidly in Hong Kong. Among these deaths, 96% occurred in persons aged ≥60 years; within this age group, the risk for death was 20 times lower among those who were fully vaccinated compared with those who were unvaccinated.