#16,776
While influenza stubbornly continues to hang on - albeit at low levels - here in the United States (see CDC FluView Report), the Southern Hemisphere's flu season is getting an early start, particularly in Queensland Australia.
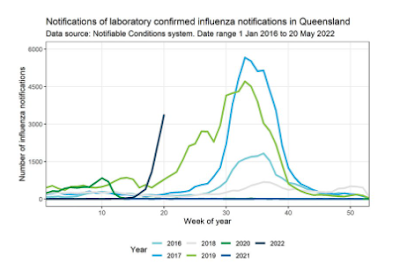
The above chart - posted overnight by Queensland Premier Annastacia Palaszczuk on her twitter account, shows an early and steep rise in influenza in her state, prompting the following announcement.
The most recent influenza report from the Australian Department of Health only spans the two weeks ending May 8th, 2022, but provides the following key messages.
Activity
- Influenza-like-illness (ILI) activity in the community in 2022 has increased since March following the decrease in activity reported in mid-February.
- In the year to date in 2022, there have been 10,599 notifications to the National Notifiable Diseases Surveillance System (NNDSS) in Australia, of which 7,173 notifications had a diagnosis date this fortnight—three times higher than notifications in the previous fortnight.
- From mid-April 2022, the weekly number of notifications of laboratory-confirmed influenza reported in Australia has exceeded the 5 year mean.
Severity
- There is no indication of the potential severity of the 2022 season at this time.
- In the year to date, of the 10,599 notifications of laboratory-confirmed influenza, no influenza-associated deaths have been notified to the NNDSS.
- There have been 153 hospital admissions due to influenza, including seven ICU admissions, reported across sentinel hospitals sites since commencement of seasonal surveillance in April 2022.
Impact
- There is no indication of the potential impact of the 2022 season on society at this time.
At-risk populations
- In 2022 to date, people aged 15–24 years and children aged younger than 10 years have the highest influenza notification rates.
Virology
- To date, 96.5% of notifications of laboratory-confirmed influenza to the NNDSS were influenza A, of which 91.3% were influenza A(unsubtyped), 2.0% were influenza A(H1N1), and 6.8% were influenza A(H3N2). Influenza B accounted for 0.2% of notifications, and 3.3% were untyped.
Vaccine match and effectiveness
- Of the 259 samples referred to the WHOCC to date, all influenza A(H1N1) and 98% of influenza A(H3N2) samples were characterised as antigenically similar to the corresponding vaccine components, while the influenza B/Victoria sample was characterised as antigenically dissimilar.
- It is too early to assess vaccine match and effectiveness for this season.
After two years of COVID-disrupted flu activity, community immunity to seasonal influenza is believed to be fairly low. At the same time, surveillance of flu's evolution around the world has been dramatically reduced (see ECDC Influenza Characterisation Report - Feb. 2022), increasing the chances we could be blindsided by a `drifted' virus (again) this year.
The Southern Hemisphere's flu season doesn't always tell us what kind of flu season we can expect next fall, but it can often provide us with some valuable early data.
Additionally, the vaccine they are deploying now is nearly identical to the vaccine we'll be using next fall, and that may give us some early insight into its effectiveness.
Just as importantly, we have yet to see how a full-blown flu season interacts with the SARS-CoV-2 pandemic virus. Preliminary studies (see The Lancet: SARS-CoV-2 Co-infection With Influenza Viruses, RSV, or Adenoviruses) suggest that influenza-COVID co-infections could be relatively common, and could significantly increase winter mortality.

While seasonal flu may seem rather mundane compared to hot topics like COVID, Monkeypox, unexplained Acute Hepatitis in Children, and avian flu - it's negative impact on our health, society, and economy each year is enormous - and we ignore it at our own peril.