#17,000
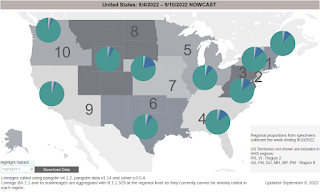
BA.5 has been the dominant subvariant in the United States for the past 3 months, and according the CDC's latest Nowcast, continues to account for > 87% of COVID cases over the past week.
While Alpha and Delta both held sway for roughly 6 months each, this is the longest and strongest showing for an Omicron variant we've seen to date.
BA.4.6 continues to make inroads - particularly in the Midwest and South - but still only accounts for less than 10% of cases nationwide. Interestingly, BA.2 - which had nearly disappeared a few weeks ago, appears to be making a bit of a comeback (1% of cases).
If recent history is any guide, then BA. 5 would be expected to give way to another variant eventually, but whether that will be BA.4.6, or BA.2.75 making moves in India, or something else remains to be seen.
BA.5 and BA.4 share identical spike proteins, allowing both to be covered by the new booster shot, but they differ genetically due to mutations outside of the spike gene.With BA.5/BA.4 specific boosters now available, the longer BA.5 can reign, the better.
Both are world class escape artists (see NEJM: Neutralization Escape by SARS-CoV-2 Omicron Subvariants BA.2.12.1, BA.4, and BA.5) - often able to evade prior immunity (either via vaccine or previous infection).
Resistance of SARS-CoV-2 Omicron Subvariant BA.4.6 to Antibody NeutralizationQian Wang, Zhiteng Li, Jerren Ho, Yicheng Guo, Andre Yanchen Yeh, Michael Liu, Maple Wang, Jian Yu, View ORCID ProfileZizhang Sheng, Yaoxing Huang, Lihong Liu, David D. Hodoi: https://doi.org/10.1101/2022.09.05.506628
Abstract
SARS-CoV-2 Omicron subvariants BA.4.6, BA.4.7, and BA.5.9 have recently emerged, and BA.4.6 appears to be expanding even in the presence of BA.5 that is globally dominant. Compared to BA.5, these new subvariants harbor a mutation at R346 residue in the spike glycoprotein, raising concerns for further antibody evasion. We compared the viral receptor binding affinity of the new Omicron subvariants with BA.5 by surface plasmon resonance. We also performed VSV-based pseudovirus neutralization assays to evaluate their antigenic properties using sera from individuals who received three doses of a COVID-19 mRNA vaccine (boosted) and patients with BA.1 or BA.2 breakthrough infection, as well as using a panel of 23 monoclonal antibodies (mAbs).
Compared to the BA.5 subvariant, BA.4.6, BA.4.7, and BA.5.9 showed similar binding affinities to hACE2 and exhibited similar resistance profiles to boosted and BA.1 breakthrough sera, but BA.4.6 was slightly but significantly more resistant than BA.5 to BA.2 breakthrough sera.Moreover, BA.4.6, BA.4.7, and BA.5.9 showed heightened resistance over to a class of mAbs due to R346T/S/I mutation. Notably, the authorized combination of tixagevimab and cilgavimab completely lost neutralizing activity against these three subvariants.
The loss of activity of tixagevimab and cilgavimab against BA.4.6 leaves us with bebtelovimab as the only therapeutic mAb that has retained potent activity against all circulating forms of SARS-CoV-2. As the virus continues to evolve, our arsenal of authorized mAbs may soon be depleted, thereby jeopardizing the wellbeing of millions of immunocompromised persons who cannot robustly respond to COVID-19 vaccines.
A little more than a year ago - when many world leaders were touting the `imminent end of the pandemic' - the UK's SAGE (Scientific Advisory Group for Emergencies) on COVID released a series of detailed reports on the SARS-CoV-2 pandemic, and where they thought things might go from there.
Their `worst-case' scenario (#1 - a much more severe variant emerges) has, thankfully, not come to pass. But scenario #2 (decreasing vaccine effectiveness) and scenario #3 (Emergence of a drug resistant variant) are both grim realities a year later.
While our pharmaceutical cupboard isn't completely bare, treatment options have decreased markedly over the past 9 months, and newer variants could further erode our medical armamentarium against COVID.
As much as people want BA.5 to be COVID's last hurrah, the virus continues to mutate and evolve in unpredictable ways, and we need to be prepared to deal with additional challenges in the future.

