#17,660
With HPAI H5N1 raging around the world in wild and migratory birds, and spilling over at record rates into mammals (see here, here, here, and here) there are growing concerns that this avian flu might someday adapt well enough to humans to spark a pandemic.
While there are scores of strains of H5N1, with differing levels of virulence, of the 878 known human infections, 458 (52%) have proven fatal. Taking into account the (unknown) number of mild infections never detected, its actual CFR (Case Fatality Rate) is likely far lower, but would probably still be substantial.
The 1918 pandemic reportedly had a 2.5% CFR, yet it killed between 50 and 100 million people, meaning H5N1 would have to have to shed a lot of its apparent CFR to be comparable.
Understanding how H5N1 spreads and infects its hosts, its pathogenesis and true CFR, and what currently available medical countermeasures might lower its impact, are all ongoing topics of research.
Long time readers of AFD will remember back in 2009, we took a deep dive (a 3-blog-series) into a study of the innate immune response of primates challenged with H5N1. The authors compared its impact to the 1918 flu virus, writing:
While both 1918 reassortant viruses also were highly pathogenic, the H5N1 virus was exceptional for the extent of tissue damage, cytokinemia, and interference with immune regulatory mechanisms, which may help explain the extreme virulence of HPAI viruses in humans.
Today's study, published in the journal Cell, raises (once again) the issues of immune imprinting, the importance of viral load, and raises the possibility that previous flu vaccination might reduce the impact of H5N1 infection.
There is a lot to unpack, and a number of caveats, including:
- First, the H5N1 virus used in this study (A/Vietnam/1203/2004) is from a much older, and far different clade, than what circulates today.
- Second, the pre-exposure vaccination schedule used on these macaques (3 adjuvanted QIV within 2.5 months) is far more aggressive than normally used in humans.
- And finally - unlike these macaques - by early in life most humans are assumed to have had a series of influenza and/or flu vaccine exposures, which may have imprinted their immune systems to recognize some flu strains better than others (see PLoS Path.: Childhood Immune Imprinting to Influenza A).
The link, abstract, and some excerpts from the discussion follow (although you'll want to read the report in full). I'll return after the break with more.
Refined semi-lethal aerosol H5N1 influenza model in cynomolgus macaques for evaluation of medical countermeasures
Masaru Kanekiyo 1 ς, Rebecca A. Gillespie 1, Morgan Midgett 2, Katherine J. O’Malley 2 7, Connor Williams 2, Syed M. Moin 1, Megan Wallace 3 8, Luke Treaster 4, Kristine Cooper 5, Hubza Syeda 1, Gwenddolen Kettenburg 3 9, Hasala Rannulu 2 10, Tabitha Schmer 2, Lucia Ortiz 6, Priscila Da Silva Castanha 3, Jacqueline Corry 3 11, Mengying Xia 2 12, Emily Olsen 2 13, Daniel Perez 6, Gabin Yun 4…Douglas S. Reed 2
https://doi.org/10.1016/j.isci.2023.107830Get rights and content
Under a Creative Commons license
Highlights
- Refined the #H5N1 aerosol macaque model of lethal ARDS
- A lower dose still triggered fever, severe respiratory disease, and death
- Three doses of quadrivalent influenza vaccine plus adjuvant protected against death
- Pre-challenge neutralizing antibody titers correlated with disease
ABSTRACT
Highly pathogenic avian influenza A H5N1 viruses cause high mortality in humans and have pandemic potential. Effective vaccines and treatments against this threat are urgently needed.
Here, we have refined our previously established model of lethal H5N1 infection in cynomolgus macaques. An inhaled aerosol virus dose of 5.1 log10 pfu induced a strong febrile response and acute respiratory disease, with four out of six macaques succumbing after challenge.
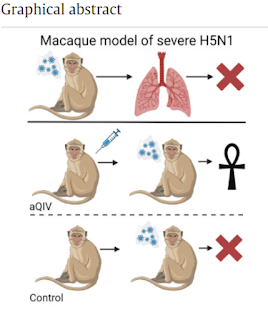
Vaccination with three doses of adjuvanted seasonal quadrivalent influenza vaccine elicited low but detectable neutralizing antibody to H5N1. All six vaccinated macaques survived four times the 50% lethal dose of aerosolized H5N1, while four of six unvaccinated controls succumbed to disease.
Although vaccination did not protect against severe influenza, vaccinees had reduced respiratory dysfunction and lower viral load in airways compared to controls. We anticipate that our macaque model will play a vital role in evaluating vaccines and antivirals against influenza pandemics.
(SNIP)
DISCUSSION
Sporadic yet recurring outbreaks in humans as well as frequent spillovers to mammalian species of HPAI H5N1 virus pose serious concerns for a potential influenza pandemic in the future. Efforts to develop vaccine candidates that provide broader protection against future pandemic influenza viruses are critical to protect global public health.
Concomitantly, efforts to develop model systems capable of evaluating vaccine and drug candidates are also essential as efficacy against pandemic influenza cannot be evaluated in human clinical trials.
Here, we validated the use of aerosol challenge with HPAI H5N1 virus in the cynomolgus macaque model as a surrogate for human pandemic influenza virus infection associated with high morbidity and mortality and showed that repeated vaccination with aQIV could offer protection from mortality caused by H5N1 virus.
We had previously established that in cynomolgus macaques, high doses of aerosolized H5N1 induced a fulminant, lethal viral pneumonia 25. Infection triggered a cytokine storm and activation of the inflammasome, triggering pyroptosis of alveolar epithelial cells and disruption of the epithelial barrier 32.
We sought to evaluate here whether lower doses would extend the disease course and alter the outcome. At the lowest doses tested we still saw evidence of infection and viral replication but only mild disease.
We were able to establish an LD50 for aerosolized H5N1; macaques infected around this dose developed severe respiratory disease and two-thirds succumbed to disease and were humanely euthanized within 4-6 days. Hence,
(SNIP)
Although HA of the HPAI H5N1 virus is quite different from that of seasonal human H1N1 viruses, both H5 and H1 subtypes belong to group 1 influenza viruses, and there are conserved HA epitopes between these viruses including the stem region.
Current seasonal influenza vaccines did not elicit protective immunity against lethal H5N1 challenge in mice or ferrets even when co-administered with adjuvant multiple times 28 , potentially due to the inability of these animals to efficiently respond to the HA stem epitope which is conserved among group 1 HA subtypes. In contrast, macaques are capable of generating neutralizing antibodies targeting the HA stem epitope 30,31 , and those antibodies could provide prophylactic protection against H5N1 in mice 28,31 .
In this study, we showed that the aQIV-vaccinated macaques were protected against mortality caused by the aerosolized H5N1 infection. H5N1 virus neutralizing antibody titers did correlate with a reduction in both fever and virus titer in BAL. Given the weak neutralizing and HA-binding antibody titers to H5N1, it is possible that T cell responses might also be playing a role for the level of protection seen, similar to what has been suggested for how ancestral SARS-CoV-2 vaccines still prevent hospitalization and death after infection with new variants that are poorly recognized by anti-spike antibodies 36,37 .
Alternatively, immune responses to other non-HA antigens such as neuraminidase may be playing a role in the protection against death.
In summary, our refined semi-lethal aerosolized H5N1 macaque infection model will be useful not only to study the pathogenesis of this important virus but also to evaluate candidate vaccines and therapeutics. In the wake of the coronavirus pandemic and a new emphasis on pandemic preparedness, extension of this macaque model to explore virulence of other influenza subtypes/strains and efficacy of medical countermeasures should be a high priority.
Given the limitations of this study we can't state much with certainty, except perhaps that the initial viral load matters when it comes to the severity, and outcome, of H5N1. According to this report, a lower viral dose . . . . resulted in comparatively milder disease . . . at least in macaques.
Assuming the same holds true for humans, wearing a well-fitted N95/KN95 mask might provide substantial benefits during an H5N1 pandemic.
The benefits of previous (or recent) seasonal flu vaccines are harder to quantify, and may even be influenced by the first flu virus you were exposed to as a child.
Eight years ago, in Science: Protection Against Novel Flu Subtypes Via Childhood HA Imprinting, we looked at research which suggested the influenza HA Group type (1 or 2) you are first exposed to makes a significant, and lasting, impression on your immune system
- Those born prior to the mid-1960s were almost certainly first exposed to Group 1 flu viruses (H1N1 or H2N2)
- Those born after 1968 and before 1977 would have been exposed to Group 2 (H3N2)
- After 1977, both Group 1 and 2 viruses co-circulated, meaning the first exposure could have been to either one.
What we are learning is that influenza viruses, and our varied immune responses to them, are far more complex than we could have imagined only a few short years ago.
Hopefully, studies like this will provide us with some modicum of an advantage when the next influenza pandemic invariably begins its world tour.

