One of the realities of science is there are far less certainties than we'd like. Facts can often have a `shelf life', and what may be thought to be true today may be proven otherwise tomorrow. Even well-mounted, contemporaneous, peer-reviewed studies may arrive at vastly different conclusions.
Over the years we've looked at a number of scientific disagreements, including:
- Last fall, in USDA Bans Import Of French Poultry Over HPAI Vaccine Concerns, we looked at conflicting views over the safety and effectiveness of using poultry vaccines to protect against H5N1.
- Over the years we've seen numerous debates over the effectiveness of different types of PPE (see MMWR: Relative Effectiveness Of Different Mask Types In Preventing COVID Infection).
- In April 2020, in When Studies Collide (COVID-19 Edition), we looked at some wildly different `conclusions' regarding the level of acquired community immunity in the UK and Austria.
- While in 2010, in When Studies Collide (Revisited), we looked at conflicting research on the efficacy of N95 respirators vs surgical masks, the effectiveness of Tamiflu (r) in treating influenza, and the dueling studies over whether seasonal flu shots can reduce the risk of heart attack and strokes.
Outliers, however, can sometimes reveal flaws in other studies.
Covid-19 infection causes several neurological diagnoses
In the general Danish population, several neurological disorders were diagnosed after infection with covid-19. This is shown by a new large study from the Statens Serum Institut, which included just under 1.8 million infected Danes.Last edited on February 20, 2024
In a new large registry-based study, researchers from the Statens Serum Institut (SSI) have investigated the connection between infection with covid-19 and the risk of developing psychiatric and neurological disorders in the time after the acute covid-19 disease was over. The study shows that there were slightly more neurological diagnoses than expected among the Danes who had previously been infected.
In the period from March 2020 to January 2023, the researchers followed 3.2 million Danes over the age of 12. During this period, almost 1.8 million of the participants were infected with covid-19. After the acute covid-19 disease was over, the researchers calculated how many hospital contacts with psychiatric and neurological diagnoses there were in the subsequent period, and compared this with the frequency of non-covid-19 infected people. In the study, they looked at 11 psychiatric and 30 neurological disorders.
"We did not observe more psychiatric diagnoses, but slightly more neurological diagnoses than expected. What takes up most of the figures are things like headaches and sleep disorders, and then of course the well-known disorders of the sense of taste and smell. We did not see correlations with fatigue and exhaustion or dementia, which are some of the things that have been highlighted from other studies," says professor and head of department Anders Hviid, who led the study.
Doubt about long-term effects on the nervous system
Covid-19, like other infectious diseases, can be a tough time for the body. There is also some research that points in the direction that the brain and nervous system can be affected in connection with the acute infection. But it is still unclear how the nervous system is affected for a long time after infection with covid-19.
American studies in particular have pointed to significantly increased risks for both psychiatric and neurological disorders for a long time after infection. But these studies often look at special population groups, for example former veterans from the US military, and it is unclear whether these results can be transferred to the general Danish population. In the new Danish study, however, there is nothing to indicate significantly more diagnoses for the Danes who have been infected.
"We saw 5% more neurological diagnoses among those previously infected, and this is probably at a level where we can say that Covid-19 does not cause more neurological late effects than so many other diseases do. But it is important to emphasize that the 5% covers large fluctuations. We saw that the hospitalized patients with severe covid-19 had significantly more psychiatric and neurological diagnoses, and we saw that infection with the omicron variant and vaccinated infected were associated with slightly fewer," says Anders Hviid.
The study has just been published in the respected scientific journal Neurology.
The full study is behind a paywall at the link below.
SARS-CoV-2 Infection and Risk of Postacute Psychiatric and Neurologic Diagnoses
A Nationwide Danish Cohort Study
Nete M. Nielsen, MD, MSc, PhD, Lampros Spiliopoulos, MSc https://orcid.org/0000-0001-9668-3587, Jørgen V. Hansen, MSc, PhD, Poul Videbech, MD, DrMedSci, and Anders Hviid, MSc, DrMedSci
Due to their relatively small population (5.8 million) and a well-monitored universal healthcare system, Denmark's ability to track and report on COVID is among the best in the world. Exactly why they should report fewer neurological complications from COVID infection is a bit of a mystery.
EID Journal: Estimates of Incidence and Predictors of Fatiguing Illness after SARS-CoV-2 Infection
Neurology: Association Between Guillain-Barré Syndrome and COVID-19 Infection and Vaccination
Viruses Review: Cerebrovascular Disease in COVID-19
Nature: Long-term Effects of SARS-CoV-2 Infection on Human Brain and Memory
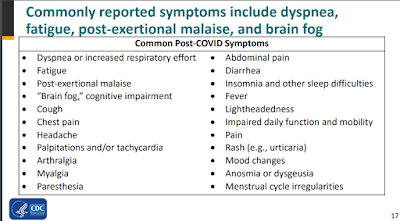
While it isn't clear how many of those cases were due to `neurological' symptoms, fatigue, and cognitive problems are among the most frequently cited `long COVID' symptoms.