#18,045
While HPAI H5Nx currently has most of our attention, we continue to watch a number of other emerging disease threats, including Mpox (formerly Monkeypox) which continues to evolve as it spreads both in endemic regions of Africa, and around the world.
Although the global health emergency for the international spread of a new clade (IIb) of Mpox ended nearly a year ago, we continue to see sporadic infections around the globe, while a more dangerous clade I mpox virus continues to rage (>12,000 cases in 2023) in the DRC.
In November of last year, the WHO Reported the 1st Confirmed Cluster Of Sexually Transmitted MPXV Clade 1 in the DRC, warning that `The risk of mpox further spreading to neighbouring countries and worldwide appears to be significant.'
The changing epidemiology and genetic evolution of mpox clade I in central Africa has sparked a number of risks assessments over the past few months, including:
CDC HAN Advisory #00501: Mpox Caused by H-2-H Transmission with Geographic Spread in the Democratic Republic of the Congo
ECDC Risk Assessment On Transmission & Spread of Clade I Mpox From The DRC
Two months ago a study was published Eurosurveillance: Ongoing Mpox Outbreak in South Kivu Province, DRC Associated With a Novel Clade I Sub-lineage, which contained the first genomic analysis of samples from a previously unaffected region of the DRC (the city of Kamituga).
That study revealed a novel clade I sub-linage had emerged - most likely from a zoonotic introduction - with changes that may render current CDC tests unreliable.
Three weeks ago, in Preprint: Sustained Human Outbreak of a New MPXV Clade I Lineage in Eastern Democratic Republic of the Congo, we saw a further analysis, which called for this new lineage to be named Clade Ib, and warned of its potential to spread globally.
Whether it is the international spread of the classic clade I virus, the spread of this new (proposed) Clade Ib strain, or a resurgence of the milder clade IIb clade which began its world tour two years ago, the threat from mpox has not gone away.
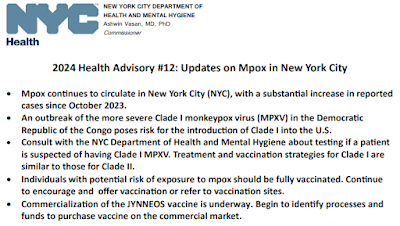
On Friday, May 3rd the New York City Health Department published the following HAN (Health Alert Network) Advisory citing increasing numbers of Mpox cases reported in the city, and the concerns over the introduction of these more dangerous clades of the virus.
I've only posted some excerpts, so follow the link to read the release in its entirety. I'll have a bit more on the JYNNEOS vaccine after the break.
• Mpox continues to circulate in New York City (NYC), with a substantial increase in reported cases since October 2023.
• An outbreak of the more severe Clade I monkeypox virus (MPXV) in the Democratic Republic of the Congo poses risk for the introduction of Clade I into the U.S.
• Consult with the NYC Department of Health and Mental Hygiene about testing if a patient is suspected of having Clade I MPXV. Treatment and vaccination strategies for Clade I are similar to those for Clade II.
• Individuals with potential risk of exposure to mpox should be fully vaccinated. Continue to encourage and offer vaccination or refer to vaccination sites.
• Commercialization of the JYNNEOS vaccine is underway. Begin to identify processes and funds to purchase vaccine on the commercial market.
May 3, 2024
Dear Colleagues,
Mpox continues to circulate in New York City (NYC). Overall, the number of cases is low compared to the 2022 outbreak, but there have been increases in cases since October 2023. This, along with the large outbreak of the more severe Clade I monkeypox virus (MPXV) in the Democratic Republic of the Congo, highlight the need for ongoing vigilance, especially approaching the summer when increased transmission may occur.
The U.S. continues to see only Clade II cases. Reported case numbers in NYC were relatively low for most of 2023, ranging from two to 20 cases per month between January and September. Since October, there has been an increase to an average of 36 cases per month, with a peak case count of 51 cases in January 2024. Of the 256 cases from October 2023 through April 15, 2024:
• 73% (188) were not vaccinated or had received only one dose.
• 94% were among men who have sex with men.
• Most were Black or Hispanic and between the ages of 25-44.
• Most were mild; ten (3.9%) people were hospitalized.
Clade I Outbreak in the Democratic Republic of the Congo
There is an outbreak of concern of Clade I MPXV in the Democratic Republic of the Congo. There have been no reported cases of Clade I in the U.S. and no evidence of transmission outside of endemic countries of Central Africa. However, it is possible that Clade I could be introduced into the U.S. by a traveler to the Democratic Republic of the Congo or other endemic countries, or with epidemiological links to those regions.
Clade I appears to be more transmissible and cause more severe disease. Isolation vaccination (JYNNEOS, ACAM2000), and treatment (e.g., tecovirimat, brincidofovir, vaccinia immune globulin intravenous) strategies used for Clade II infections are expected to be effective for Clade I infections.
Vaccination Update
People with potential risk of exposure to mpox should receive two doses of the JYNNEOS vaccine to be fully vaccinated. It is estimated that only one in four people recommended to receive the vaccine in the U.S. are fully vaccinated. Increasing vaccine uptake is essential to preventing infections and severe disease.
On April 1, 2024, the JYNNEOS vaccine began transition to the commercial market, though no cost federal supplies are available until early summer 2024. JYNNEOS vaccine will be made available through the Vaccines for Children (VFC) Program (for eligible adolescents), likely within a few months of commercialization.
Recommendations for health care providers
1) Testing
• Given mild signs and symptoms reported by most cases since the 2022 outbreak, maintain a low threshold for mpox testing to reduce the potential for missed cases. Testing should be provided to any individual who requests it and has a sore or skin lesion that can be swabbed.
• Refer to the GOALS Framework for Sexual History Taking in Primary Care to assess testing needs and facilitate the patient-provider relationship by normalizing discussions about sexual health and behavior as a routine part of health care.
• Submit mpox specimens to a commercial or facility-based laboratory that has been approved to conduct mpox testing by New York State. If testing is not feasible, call the NYC Department of Health and Mental Hygiene (Health Department) Provider Access Line at 866-692-3641 to arrange for testing, following the NYC Public Health Laboratory specimen collection guidelines.
• Be alert to the possibility of Clade I MPXV and need for specimen collection for people with symptoms and a history of travel or epidemiological links to a region of endemicity, including the Democratic Republic of the Congo, within 21 days of symptom onset.
• If Clade I MPXV is suspected, call the Provider Access Line at 866-692-3641 for immediate consultation and to arrange for testing by the Centers for Disease Control and Prevention (CDC) (currently, only CDC can test for Clade I).
2) Vaccination
• Continue to encourage vaccination for individuals for whom it is recommended and especially those with a higher risk of mpox complications (e.g., people with advanced HIV or other severe immunocompromise).
• Advise those who have not yet received a second vaccine dose to do so as soon as possible, regardless of how much time has passed since their first dose.
• Start to identify processes and funds for ordering JYNNEOS on the commercial market. • Order no-cost vaccine by emailing poxvax@health.nyc.gov. The NYC Health Department anticipates being able to fulfill requests until early summer 2024.
• If you do not offer vaccination, refer to vaccinefinder.nyc.gov to find a vaccination site.
Complicating matters, recent studies have suggested that the effectiveness of the JYNNEOS vaccine (approved in 2019) wanes significantly between 1 and 12 months, even when a person has received two doses.
Five weeks ago, in ECCMID 2024 Study: Mpox (monkeypox) Antibodies Wane Within A Year of Vaccination) we looked at a study by researchers from Erasmus MC in Rotterdam that found:
. . . recipients of the 2-Dose JYNNEOS/ IMVANEX/ IMVAMUNE mpox vaccine who did not receive a childhood smallpox vaccination (discontinued in the 1970s) experienced substantial drops in their immune response after 12 months.
Another presentation, released at roughly the same time from Sweden (see Immune response to MPXV wanes rapidly after intradermal vaccination with MVA-BN (Jynneos)) found an even quicker loss (> 28 days) of detectable neutralizing antibodies after the second vaccination, writing:
Our findings corroborate previous data showing that intradermal MVA-BN vaccination results in neutralizing antibodies only in a proportion of vaccinees, and that a significant decline occurs already during the first months post-vaccination. Immunity after MPXV infection mounts a higher and more robust neutralizing response. In conclusion, the findings merits the study of booster doses.
Immunity is based more than just detectable neutralizing antibodies, and anecdotal reports suggest the vaccine provides significant protection, but boosters may be required sooner than originally planned (see ACIP Evidence to Recommendations for Use of JYNNEOS (orthopoxvirus) Vaccine Booster Every 2 Years).
While it remains to be seen whether the two (known) clade I strains follow clade IIb out of Africa, the virus continues to mutate and evolve, and will remain a tangible threat unless and until concerted efforts are made to contain it at its source.