#18,813
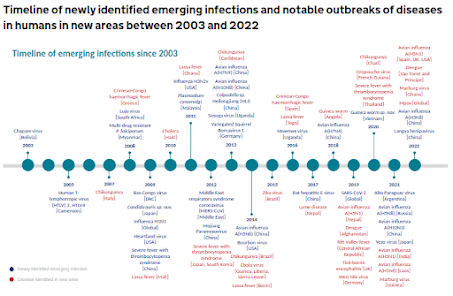
While novel influenza A has long been considered the greatest pandemic threat to humans, eight years ago the WHO released a short list (n=8) of priority diseases (see WHO List Of Blueprint Priority Diseases) - that in their estimation - had the potential to spark a public health emergency and were in dire need of accelerated research:In 2020, a variant of #4 on their list (SARS-CoV-2) sparked the worst pandemic in a century. Meanwhile, we've continued to see sporadic outbreaks of many of the others on the list.
- Crimean-Congo haemorrhagic fever (CCHF)
- Ebola virus disease and Marburg virus disease
- Lassa fever
- Middle East respiratory syndrome coronavirus (MERS-CoV) and Severe Acute Respiratory Syndrome (SARS)
- Nipah and henipaviral diseases
- Rift Valley fever (RVF)
- Zika
- Disease X
Last summer the WHO unveiled an expanded 38-page Pathogens Prioritization report, increasing the number of priority pathogens to more than 30. Additions included 7 different influenza A subtypes (H1, H3, H3, H5, H6, H7, and H10), and 5 bacterial strains that cause cholera, plague, dysentery, diarrhea and pneumonia.
In 2010's Influenza: The Once and Future Pandemic, authors Jeffery K Taubenberger & David M Morens wrote: `Influenza pandemics have been reported for at least 500 years, with inter-pandemic intervals averaging approximately 40 years.'
But, as the statistician who learned to his cost while attempting to ford a river that was - "on average, only 3 feet deep" - there are sometimes outliers.
The 1957 (H2N2) and 1968 (H3N2) pandemics were only separated by a little over a decade, and more recently - after two close calls with coronaviruses (SARS & MERS) - COVID proved that non-influenza A viruses could compete on a world stage.
The world we know is changing:
- Our global population is 3 times greater today than when I was born (1954). That year, roughly 58 million people traveled internationally by air, while in 2025 that number is expected to approach 6 billion (a 100-fold increase)
- Our world is also growing warmer, precipitation patterns are shifting, and we've continually encroached into previously untouched rainforests, deserts, and swamps in order to create farmlands, or cities, or in search of natural resources.
- In most developed countries we now raise most livestock in CAFO's (concentrated animal feeding operations), an environment which invites the spread and evolution of new diseases.
All of which brings us to a research article, published last week in Science Advances, which attempts to identify and quantify the risks of zoonotic disease outbreaks with epidemic or pandemic potential in our continually changing world.
This research article focuses heavily on climatic and anthropogenic drivers of pandemic risk, and given the paucity of data from many regions of the globe, a large number of assumptions had to be made.
Due to its length and technical nature, I've only posted the abstract and a few excerpts. Follow the link to read it in its entirety - although fair warning - some of it requires heavy lifting.
I'll have a bit more after the break.
Assessing the risk of diseases with epidemic and pandemic potential in a changing world
Angela Fanelli , Alessandro Cescatti , Juan-Carlos Ciscar, Gregoire Dubois , Dolores Ibarreta , Rachel Lowe , Nicola Riccetti https://orcid.org/0000-0002-3178-7892, Marine Robuchon , Ilaria Capua , [...] , and Emanuele Massaro+1 authors Authors Info & Affiliations
Science Advances
23 Jul 2025
Vol 11, Issue 30
DOI: 10.1126/sciadv.adw6363
Abstract
How do human activities contribute to the emergence of zoonotic diseases that can lead to epidemics and pandemics? Our analysis of common drivers of the World Health Organization’s priority diseases suggests that climate conditions, including higher temperatures, higher annual precipitation levels, and water deficits, elevate the risk of disease outbreaks.
In addition, land-use changes, human encroachment on forested areas, increased population and livestock density, and biodiversity loss contribute to this risk, with biodiversity loss showing a complex and nonlinear relationship.
This study also presents a global risk map and an epidemic risk index that combines countries’ specific risk with their capacities for preparing and responding to zoonotic threats.
(SNIP)
The World Health Organization (WHO) maintains a list of priority diseases, namely, pathogens identified as having potential to cause severe public health emergency including epidemics and pandemics (14). This prioritization intends to guide global research efforts to better prepare for and mitigate potential zoonotic outbreaks.
The list includes COVID-19, Crimean-Congo hemorrhagic fever (CCHF), Ebola virus disease, Lassa fever, Middle East respiratory syndrome (MERS), severe acute respiratory syndrome (SARS), Marburg virus disease (MVD), Nipah virus disease (NiV), Rift Valley fever (RVF), Zika, and a placeholder for an unknown “Disease X” (14, 15).
Climate change affects the risk of these diseases, including vector-borne diseases such as RVF and Zika (16–19), and nonvector-borne diseases such as Ebola, which is affected by climate change through its effect on fruit abundance, attracting bats, and increasing the chance of human contact with infected reservoirs (20). Extreme weather events, forest fragmentation, and deforestation can also increase the risk of disease transmission, such as Lassa fever (21).Building on the above context, our study aimed to investigate the relationship between nine key human-induced drivers and the outbreak risk of WHO priority diseases, excluding COVID-19. We also developed a global risk map and an epidemic risk index that reflects each country-specific risk versus its capacity to respond to zoonotic threats.
(SNIP)
We considered nine potential drivers of the WHO priority diseases, grouped into three categories: climate factors (temperature, precipitation, and water deficit), environmental factors (human-forest proximity, biodiversity loss, livestock density, and frequency of land-use change), and population (population density). In the multivariable analysis, we also incorporated the travel time to health care facilities as a bias breaker, ensuring that the probability of disease detection influenced by the proximity of health care facilities is accounted for.
- ongoing reassortment or recombination in the wild has produced unprecedented diversity of zoonotic viruses around the globe
- reverse zoonosis (human to animal)
- long-term infections among immunocompromised individuals leading to mutations or variants
- laboratory accidents
- bio-terrorism
- growing antibiotic/antiviral resistance
- advances in synthetic biology
- and even social media driven misinformation on vaccines and science
While we should certainly endeavor to mitigate zoonotic disease risks wherever we can, the reality is, nature always bats last.
And we never know when we're approaching the bottom of the 9th inning.