# 9747
Although the MERS coronavirus has yet to be declared a PHEIC (Public Health Emergency Of International Concern), it is nonetheless a worrisome, high-mortality virus that after nearly three years - and more 1,000 cases - we still know far too little about.
Recently we’ve seen assessments from the World Health Organization (see Saudi Arabia: WHO MERS Mission Summary & WHO Summary & Risk Assessment On MERS-CoV) that discuss some of these dangerous gaps in our knowledge, and that urge the Saudis to intensify their research efforts.
Meanwhile, we’ve watched a steady increase in cases over the past couple of months, and already February of 2015 is the 4th most active MERS month on record.
While cases have only emerged from on the Arabian peninsula (KSA being the most active by far), the virus has been exported to 8 European countries, and to 13 nations beyond the Middle East.
With up to a 15 days incubation period, it is all to easy for someone to acquire the virus in the Middle East and travel while still asymptomatic anywhere in the world.
KSA: The Global hub of MERS – Credit ECDC
Accordingly the ECDC issues updated Rapid Risk Assessments from time to time (the last one was in January) where they review the epidemiology of the virus, and discuss the degree of threat the virus poses to the EU. The consensus to date remains:
Although importation of MERS-CoV cases to the EU remains possible, the risk of sustained human-to-human transmission in Europe remains very low.
EA few excerpts from today’s report follows, but the entire PDF is well worth downloading an reviewing.
Main conclusions and recommendations
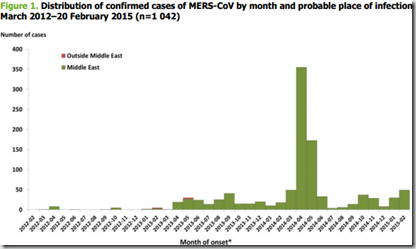
Since April 2012 and as of 20 February 2015, 1 042 cases (including 419 deaths) of Middle East respiratory syndrome coronavirus (MERS-CoV) have been reported by local health authorities worldwide.
The incidence of MERS-CoV cases has been on an increase in Saudi Arabia since December 2014. This increase parallels the increase observed in early 2014 and may be indicative of the start of a seasonal pattern. Most of the increase in the recent weeks affects Riyadh, and one third of the recent cases may have a nosocomial origin. Twelve per cent of the recent cases have reported contact with an animal or animal product. This is consistent with the transmission pattern observed in early 2014, which showed increased transmission from a primary animal source, most likely camels or camel products, amplified by nosocomial transmission.
The importation of a case in the Philippines demonstrates the possibility of importation of cases from abroad, especially in relation with healthcare workers infected while caring for patients in Saudi Arabia.
The majority of MERS-CoV cases are still reported from the Arabian Peninsula, mainly from Saudi Arabia.
The source of MERS-CoV infection and the mode of transmission have still not been confirmed.
Taking into account the latest developments with respect to MERS-CoV, ECDC’s conclusion continues to be that the MERS-CoV outbreak poses a low risk to the EU.
Because of the continued risk of cases in Europe after exposure in the Middle East, international surveillance for MERS-CoV cases remains essential. Although importation of MERS-CoV cases to the EU remains possible, the risk of sustained human-to-human transmission in Europe remains very low.
Sensitisation of healthcare staff to MERS-CoV is prudent, not only for timely detection purposes, but also in order to ensure rapid implementation of infection control measures.Worldwide situation
Since April 2012 and as of 20 February 2015, 1 042 cases (including 419 deaths) of MERS-CoV have been
reported by health authorities worldwide (Figure 1).CONCLUSIONS
The large surge in infections seen in the spring of 2014 was mainly due to an outbreak in Jeddah, but driven by
an increase in primary infections [8]. A similar increase is possible in spring 2015, and public health authorities in the epicentre are currently preparing appropriate response measures. In Saudi Arabia, response activities have recently been decentralised and are now managed by the regional health departments [9].
In the EU/EEA, public health authorities are prepared for the timely detection and appropriate treatment of cases in returning travellers, should the need arise. Sensitisation of first-line healthcare staff to the fact that MERS-CoV is still circulating in the Middle East is prudent, not only for timely detection purposes, but also in order to ensure rapid implementation of infection control measures.
Taking into account the latest developments with respect to MERS-CoV, ECDC’s conclusion continues to be that the MERS-CoV outbreak poses a low risk to the EU. Because of the continued risk of the importation of cases to Europe after exposure in the Middle East, international surveillance for MERS-CoV cases remains essential. Although importation of MERS-CoV cases to the EU remains possible, the risk of sustained human-to-human transmission in Europe remains very low.