For now it appears that seasonal H1N1 has been supplanted by novel H1N1, and we are left with four flu strains (novel H1N1, H3N2, and 2 B lineages) in circulation as of the fall of 2010.
# 5015
We don’t discuss Influenza B very often, because among the influenzas, B strains are regarded as less pathogenic and more stable (and less likely to spark a pandemic) than their highly mutable cousins; influenza A.
And so most scientific research and attention is focused on the more unpredictable and dangerous A strains.
But today, we’ll make an exception because Influenza B has been in the news a little this week, including research on Influenza B and bacterial co-infections.
First, here is how the CDC describes influenza B.
Influenza Type B
Influenza B viruses are usually found only in humans. Unlike influenza A viruses, these viruses are not classified according to subtype. Influenza B viruses can cause morbidity and mortality among humans, but in general are associated with less severe epidemics than influenza A viruses. Although influenza type B viruses can cause human epidemics, they have not caused pandemics.
While considered less dangerous, that doesn’t make Influenza B unworthy of our attention.
Influenza B was first identified - almost simultaneously - by two researchers back in 1940 (Francis and Magill). Unlike the A strains, Influenza B was discovered to remain relatively stable, usually for years at a time.
It often becomes the predominant strain late in the flu season, after influenza A has peaked.
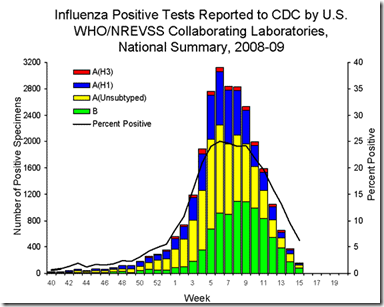
This graphic from the CDC’s 2009 FluView shows Influenza B making up about half of all positive flu samples from week 11 to week 15.
There are two lineages of influenza B that currently circulate around the world (and have since the late 1980s); the Victoria and Yamagata strain.
And each year scientists must decide . . . six months in advance . . . which of these strains to include in the next seasonal flu shot. Their record for guessing which strain will dominate has been less than stellar – missing the mark about half the time in recent years.
Which has sparked calls to formulate a quadrivalent flu vaccine – one that includes two A strains, and both lineages of the B strain each year (see Two Bs Or Not Two Bs? April 2010).
You can find an earlier but nonetheless illuminating discussion of the advantages and problems of manufacturing a quadrivalent vaccine in this CIDRAP report from January of 2009 (Experts consider 4-strain flu vaccine to fight B viruses).
Earlier this week CIDRAP reported on Sanofi’s early testing of a quadrivalent vaccine in Sanofi reports trial results for novel flu vaccines.
While having a diminished pandemic potential, and producing (generally) less severe illness, influenza B is hardly benign. It can (and does) contribute to the burden of influenza mortality and morbidity each year – particularly among children and younger adults.
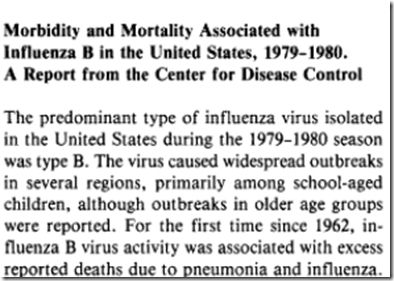
The following is an account from the Journal of Infectious Diseases, Sept 1980, describing the impact of an influenza B dominated flu season.
Today we’ve a new example of the pathogenic potential of influenza B which comes by way of a journal article from BMC Infectious Diseases.
It looks at 3 previously healthy women (with no apparent high risk factors) who developed serious pneumonia and sepsis as a result of a co-infection with influenza B.
I’ve reproduced the Abstract below. A provisional PDF of the entire article is available here. (note the typo in the first sentence: that should read 1918)
Co-infection of Influenza B and Streptococci causing Severe Pneumonia and Septic Shock in Healthy Women
Timothy Aebi , Maja Weisser , Evelyne Bucher , Hans H Hirsch , Stephan Marsch and Martin Siegemund
BMC Infectious Diseases 2010, 10:308doi:10.1186/1471-2334-10-308
Published:
27 October 2010Abstract (provisional)
Background
Since the Influenza A pandemic in 1819, the association between the influenza virus and Streptococcus pneumoniae has been well described in literature. While a leading role has been so far attributed solely to Influenza A as the primary infective pathogen, Influenza B is generally considered to be less pathogenic with little impact on morbidity and mortality of otherwise healthy adults. This report documents the severe synergistic pathogenesis of Influenza B infection and bacterial pneumonia in previously healthy persons not belonging to a special risk population and outlines therapeutic options in this clinical setting.
Case presentation
During the seasonal influenza epidemic 2007/2008, three previously healthy women presented to our hospital with influenza-like symptoms and rapid clinical deterioration. Subsequent septic shock due to severe bilateral pneumonia necessitated intensive resuscitative measures including the use of an interventional lung assist device. Microbiological analysis identified severe dual infections of Influenza B with Streptococcus pyogenes in two cases and Streptococcus pneumoniae in one case. The patients presented with no evidence of underlying disease or other known risk factors for dual infection such as age (<one year, >65years), pregnancy or comorbidity.
Conclusion
Influenza B infection can pose a risk for severe secondary infection in previously healthy persons. As patients admitted to hospital due to severe pneumonia are rarely tested for Influenza B, the incidence of admission due to this virus might be greatly underestimated, therefore, a more aggressive search for influenza virus and empirical treatment might be warranted. While the use of an interventional lung assist device offers a potential treatment strategy for refractory respiratory acidosis in addition to protective lung ventilation, the combined empiric use of a neuraminidase-inhibitor and antibiotics in septic patients with pulmonary manifestations during an epidemic season should be considered.
Bacterial pneumonia is a fairly common complication of severe influenza, but up until now has usually been associated with influenza A infections.
Here, researchers show that influenza B can also open the door for serious (and sometimes fatal) bacterial infections in previously healthy individuals.
The entire report is worth reading, particularly if you are a clinician.
The authors contend that since testing for influenza B is less common than for influenza A, it may be behind more hospital admissions than we know.
Another example that illustrates that - despite making great strides in recent years in our understanding of influenza - that we’ve still a lot to learn.