#17,116
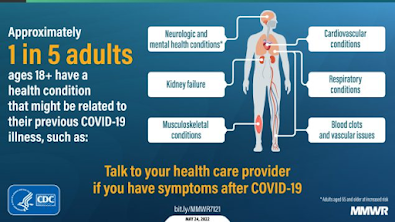
Post-COVID sequelae may include cardiovascular, renal, pulmonary, neurological, and endocrine disorders. A few (of many) studies we've looked at over the past few months include:
The Lancet: Neurological and Psychiatric Risk Trajectories After SARS-CoV-2 Infection
Over the summer, a preprint from researchers at Washington University in St. Louis (see Outcomes of SARS-CoV-2 Reinfection by Ziyad Al-Aly, Benjamin Bowe& Yan Xie) made headlines, as their findings suggested the more times one is reinfected with COVID, the greater the risk of death or post-acute sequelae.
We've previously looked at COVID studies by this team of researchers in:
Nature: Long-term Cardiovascular Outcomes of COVID-19
Nature: Long-term Neurologic Outcomes of COVID-19
Today, that preprint from last summer has been published in the journal Nature (see below), which reports that the risks of dying are doubled following reinfection with COVID, and the risks of being hospitalized are tripled.
And a 3rd, or 4th, or 5th reinfection appears to only increase those risks.
First the link, and abstract from the Nature study, followed by a press release from Washington University in St. Louis. I'll have a postscript after the break.
Acute and Postacute Sequelae Associated with SARS-CoV-2 reinfection
Nature Medicine (2022) Cite this article
Abstract
First infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is associated with increased risk of acute and postacute death and sequelae in various organ systems. Whether reinfection adds to risks incurred after first infection is unclear.Here we used the US Department of Veterans Affairs’ national healthcare database to build a cohort of individuals with one SARS-CoV-2 infection (n = 443,588), reinfection (two or more infections, n = 40,947) and a noninfected control (n = 5,334,729). We used inverse probability-weighted survival models to estimate risks and 6-month burdens of death, hospitalization and incident sequelae. Compared to no reinfection, reinfection contributed additional risks of death (hazard ratio (HR) = 2.17, 95% confidence intervals (CI) 1.93–2.45), hospitalization (HR = 3.32, 95% CI 3.13–3.51) and sequelae including pulmonary, cardiovascular, hematological, diabetes, gastrointestinal, kidney, mental health, musculoskeletal and neurological disorders.The risks were evident regardless of vaccination status. The risks were most pronounced in the acute phase but persisted in the postacute phase at 6 months. Compared to noninfected controls, cumulative risks and burdens of repeat infection increased according to the number of infections. Limitations included a cohort of mostly white males. The evidence shows that reinfection further increases risks of death, hospitalization and sequelae in multiple organ systems in the acute and postacute phase. Reducing overall burden of death and disease due to SARS-CoV-2 will require strategies for reinfection prevention.
Researchers recommend masks, vaccines, vigilance to prevent reinfection
Peer-Reviewed Publication
WASHINGTON UNIVERSITY IN ST. LOUIS
Since the COVID-19 pandemic began almost three years ago, scientists have learned that an initial infection can lead to short- and long-term health risks affecting nearly every organ system in the body. They’ve also determined that people can get COVID-19 a second or a third time, despite acquiring natural antibodies after the first infection and receiving vaccination and booster shots.
Now, a new study from Washington University School of Medicine in St. Louis and the Veterans Affairs St. Louis Health Care system shows the health consequences of reinfection. The researchers found that repeat SARS-CoV-2 infections contribute significant additional risk of adverse health conditions in multiple organ systems.
Such outcomes include hospitalization; disorders affecting the lungs, heart, brain, and the body’s blood, musculoskeletal and gastrointestinal systems; and even death. Reinfection also contributes to diabetes, kidney disease and mental health issues.
The findings are published Nov. 10 in Nature Medicine.
“During the past few months, there’s been an air of invincibility among people who have had COVID-19 or their vaccinations and boosters, and especially among people who have had an infection and also received vaccines; some people started to referring to these individuals as having a sort of superimmunity to the virus,” said senior author Ziyad Al-Aly, MD, a clinical epidemiologist at the School of Medicine. “Without ambiguity, our research showed that getting an infection a second, third or fourth time contributes to additional health risks in the acute phase, meaning the first 30 days after infection, and in the months beyond, meaning the long COVID phase.”
Additionally, the study indicated that the risk seems to increase with each infection. “This means that even if you’ve had two COVID-19 infections, it’s better to avoid a third,” Al-Aly said. “And if you’ve had three infections, it’s best to avoid the fourth.”
Limiting exposure to the virus is especially important as the U.S. heads into the winter months, with new variants emerging, mutating and already causing an upswing in infections in some parts of the country, Al-Aly said. “People should do their best to prevent repeat infections by masking, for example, getting all of their eligible boosters, staying home when sick. Also, get a flu shot to prevent illness. We really need to do our best to reduce the chance we will have a twin-demic of both COVID-19 and the flu this winter season.”
For this study, the researchers analyzed about 5.8 million de-identified medical records in a database maintained by the U.S. Department of Veterans Affairs, the nation’s largest integrated health-care system. Patients represented multiple ages, races and sexes.
The researchers created a controlled data set of 5.3 million people who did not test positive for COVID-19 infection from March 1, 2020, through April 6, 2022. Using the same time frame, the researchers also compiled a control group of more than 443,000 people who had tested positive for one COVID-19 infection, and another group 5.8 million of nearly 41,000 people who had two or more documented infections. Of the latter group, most people had two or three infections, with a small number having had four infections and no one with five or more infections.
Statistical modeling was used to examine the health risks of repeat COVID-19 infections within the first 30 days after contracting the virus and up to six months after.
The study accounted for COVID-19 variants such as delta, omicron and BA.5. Negative outcomes occurred among the unvaccinated as well as those who had received shots prior to reinfection.
Overall, the researchers found that people with COVID-19 reinfections were twice as likely to die and three times more likely to be hospitalized than those with no reinfection.
Additionally, people with repeat infections were 3½ times more likely to develop lung problems, three times more likely to suffer heart conditions and 1.6 times more likely to experience brain conditions than patients who had been infected with the virus once.
“Our findings have broad public health implications as they tell us that strategies to prevent or reduce the risk of reinfection should be implemented,” Al-Aly said. “Going into the winter season, people should be aware of the risks and practice vigilance to reduce their risk of infection or reinfection with SARS-CoV-2.”
Since the summer of 2020 we've seen a steady parade of studies and articles on the long-term detrimental impacts from COVID infection. I've listed a dozen already in this blog post, but could have easily listed dozens more.
Despite the preponderance of evidence of substantial harm, most people now dismiss COVID as a trivial illness, and point to its high survival rate - even among those hospitalized - as if that tells the whole story.
But mounting evidence shows the long-term impacts of COVID infection can be serious, and potentially deadly. It may be years before we can fully determine the impact of COVID on public health, but based on what we do know, this coronavirus remains an infection very much worth avoiding.
Which is why I'm still wearing a face mask in public, am keeping current with my booster shots, and will avoid putting myself unnecessarily in crowded, or poorly ventilated, indoor venues this winter.