#17,622
Although much of the world has taken a `If we ignore it, maybe it will go away' stance when it comes to COVID, the SARS-CoV-2 virus continues to roll the genetic dice, and will likely continue to stumble upon new ways to enhance its ability to escape immunity and transmit more efficiently (in humans, and other hosts).
Reporting by member nations to the WHO continues to deteriorate, with roughly 90% of the world's nations not regularly reporting hospitalizations, ICU admissions, or deaths.
The WHO continues to urge surveillance and reporting (below):
As countries discontinue COVID-19-specific reporting and integrate respiratory disease surveillance, WHO will continue to use all available sources to continue monitoring the COVID-19 epidemiological situation. COVID-19 continues to be a major threat and WHO urges Member States to maintain, not dismantle, their established COVID-19 infrastructure. It is crucial to sustain early warning, surveillance and reporting, variant tracking, early clinical care provision, administration of vaccine boosters to high-risk groups, improvements in ventilation, and regular communication.
Few, however, are listening. Most countries - for economic, political and societal reasons - have decreed that COVID is no longer a threat, there is no reason to treat it any differently than influenza, and that it is time to move on.
And I get it.
COVID isn't going to go away, and new waves are inevitable. The world can't stay at full alert indefinitely. And people are fed up with taking precautions, getting vaccines, and living under the constant `threat' of the next wave.
Added to that, China has proved that there is little downside to hiding millions of COVID cases, and likely millions of deaths. There are no penalties, no international sanctions. It doesn't change anything on the ground, and the less said, the better it is for their economy and ruling party.
And that attitude has spread globally. Which is why only 1 in 10 countries regularly report COVID hospitalization, ICU admissions, or deaths. And why we rarely hear about MERS-CoV cases from the Middle East or human infections with avian flu from around the globe.
This is one of those plans that works . . . until it doesn't.
As long as a new, and highly transmissible disease doesn't emerge, we can party like its 2019. And it may be years before another pandemic threat comes along. And even if it does, the odds are it will emerge in somebody else's back yard.
Luckily, there are still a few pesky entities out there that insist on to peering into the fog, looking for signs of the next emerging threat; the WHO, ECDC, HKHSA, our own CDC, and researchers from universities from around the world, to name a few.
Yesterday, we saw the WHO elevate the recently discovered BA.2.86 COVID variant to VUM (Variant Under Monitoring) status, while at the same time the ECDC released an Epidemiological Update on the recent rise in XBB.1.5-like lineages carrying the F456L mutation.
At this point, there is no evidence that this F456L mutation increases the severity of disease from COVID, but it does appear linked to increased transmissibility. And with infection rates rising again - both in Europe and in the United States - researchers are taking a closer look.
Some excerpts from the Epidemiological update follow, after which I'll have a brief postscript. Follow the link to read it in its entirety.
ECDC classifies XBB.1.5-like lineages with the amino acid change F456L as variants of interest following an increase in SARS-CoV-2 transmission in EU/EEA countries and abroad
Epidemiological update
17 Aug 2023
In 2023, after several months of very low rates of infection, coronavirus disease 2019 (COVID-19) transmission has started to increase in some EU/EEA countries. Although this has coincided with increasing detections of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) XBB.1.5-like lineages carrying the F456L mutation, there are other drivers that can contribute to the increasing transmission rates. This includes large gatherings during seasonal holidays and lower levels of immunological protection against infection after several months of very low disease incidence. There is currently no sign of increased hospitalisations or pressures on healthcare systems.
ECDC classified XBB.1.5-like lineages with the additional amino acid change F456L as variants of interest (VOI) due to a rapid increase in the proportion of these variants presently in circulation, which may have immune-escape properties compared to the variants which were previously in circulation.
Based on what is observed in countries outside the EU/EEA, it is likely that F456L variants will contribute to increased transmission in the coming weeks. However, it is unlikely that the resultant levels of severe disease will reach those of similar peaks previously observed during the COVID-19 pandemic. It is also unlikely that F456L variants are associated with any increase in infection severity compared to the previously circulating variants, or reduction in vaccine effectiveness against severe disease.
However, as for other SARS-CoV-2 variants, older individuals and those with underlying conditions could develop severe symptoms if infected.
The completeness and timeliness of epidemiological and virological COVID-19 surveillance data has decreased in the last year, which affects the ability to make an assessment for all EU/EEA countries. Member States are encouraged to expand their use of, and report data from well-designed, representative population-based surveillance in primary and secondary care to monitor trends in transmission and severe disease by time, place, and person, in a timely manner. Where possible, all SARS-CoV-2-positive specimens from representative surveillance systems should be sequenced and reported to the Global Initiative on Sharing All Influenza Data (GISAID) and/or The European Surveillance System (TESSy) to facilitate the assessment of circulating variants.
Adherence to national vaccination schedules is essential to protect people at high risk for severe disease and death. Countries should assess their readiness to identify target groups and conduct timely COVID-19 vaccination campaigns. In addition, communication campaigns aimed at the public and healthcare professionals are deemed necessary to reach high-risk groups and inform them of the importance to stay up to date with vaccination.
XBB.1.5-like + F456L variant
As of 10 August 2023, ECDC classified all XBB.1.5-like lineages with the additional spike protein change F456L as SARS-CoV-2 variants of interest (VOI). The reasons for this classification are: a) the rapid increase in the proportion of this mutation in the positive samples from EU/EEA countries, b) a slight increase in the epidemiological indicators of community transmission, and c) the mutation is predicted and verified by a preliminary in-vitro study to contribute to immune escape, compared to the previously circulating variants [1].
So far there is no evidence that F456L variants meet any of the criteria for variants of concern (VOC), i.e. moderate to high evidence of the variant being associated with an increase in infection severity, a risk for compromising the healthcare capacity in the EU/EEA, or a reduction in vaccine effectiveness (Figure 1). ECDC SARS-CoV-2 variant classification criteria and recommended actions for EU/EEA Member States are outlined on the ECDC variant webpage [2,3].
Figure 1. Variant classification matrix for variants of interest (VOI): XBB.1.5-like + F456L
The mutation is also increasing globally, with the World Health Organization (WHO) classifying EG.5, which is the most prevalent lineage with this mutation, as a VOI as of 9 August 2023 [4] and the United Kingdom Health Security Agency (UKHSA) classifying EG.5.1 as a variant as of 31 July 2023 [5]. ECDC classifies EG.5 within the group of lineages carrying F456L, since all 456L-lineages exhibit elevated growth rates, and the likely source of the elevated growth rate is mainly the F456L change itself.
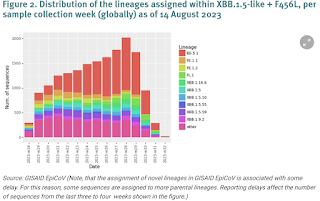
The XBB.1.5-like lineages with F456L are characterised by spike protein receptor-binding domain changes F456L, N460K, S486P, and F490S. The XBB.1.5-like umbrella already comprises several distinct lineages which are all descendants from the recombinant lineage XBB that emerged and became successful in late 2022. Among these, there are XBB.1.5, XBB.1.9.1, XBB.1.9.2, XBB.1.16, and XBB.2.3. Several different sub-lineages within these have now acquired the additional spike protein change F456L which currently seems to confer a selective advantage over the previously circulating variants. Among these lineages, there is FE.1, which rose to high proportions close to dominance in Brazil in May 2023, but did not have wider success globally. There is also EG.5, which is now the most common lineage within the F456L group, both globally and in the EU/EEA (Figure 2).
It continues to circulate in non-human as well as human hosts, repeated infections have been linked to `Long COVID' and worse outcomes, and recombination with other coronaviruses is theoretically possible (see Nature: CoV Recombination Potential & The Need For the Development of Pan-CoV Vaccines).
As we've seen from the WHO, the ECDC is also imploring members to expand surveillance and reporting, warning that reduced reporting `. . . affects the ability to make an assessment for all EU/EEA countries.'
After every public health crisis, there are always a spate of scholarly articles about `lesson's learned' from the response. The assumption is that we glean the `right lessons' from the experience, and come out better prepared.