#18,132
Not quite 5 months ago, in China NHC Statement: A Fatal Case of H3N2 and H10N5 Mixed Infection Discovered in Zhejiang Province, we learned of the first known human infection with avian H10N5, in a 62-year-old woman who was concurrently infected with seasonal H3N2.
Cases such as this, while believed rare, probably occur more often than we know, as it requires a bit of luck for them to be detected and/or reported. Mild or moderate infections - or even fatal ones in facilities or regions with less thorough testing - are unlikely to be picked up by surveillance.The patient died in mid-December, and it was only through a combination of luck and a policy of retrospectively testing samples from fatal flu cases in China, that this case was identified 7 weeks after her initial hospitalization, and 5 weeks after her death.
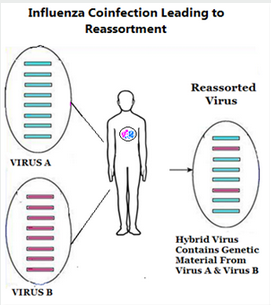
Co-infections in humans - or in any other susceptible host (birds, pigs, etc.) - are a concern because it can allow two (or more) influenza viruses to swap genetic material (reassort) producing a hybrid virus (see graphic at top of blog).
And twice in my lifetime (1957 and 1968), we've seen that happen.
- The first (1957) was H2N2, which According to the CDC `. . . was comprised of three different genes from an H2N2 virus that originated from an avian influenza A virus, including the H2 hemagglutinin and the N2 neuraminidase genes.'
- In 1968 an avian H3N2 virus emerged (a reassortment of 2 genes from a low path avian influenza H3 virus, and 6 genes from H2N2) which supplanted H2N2 - killed more than a million people during its first year - and continues to spark yearly epidemics more than 50 years later.
In mid-February, in WHO Risk Assessment On Co-infection With H10N5 & Seasonal H3N2 in China, we learned that the woman had exposure to live poultry, and poultry samples also tested positive for H10N5.
No other cases were discovered during the epidemiological investigation, however, that was conducted nearly 2 months after the woman's initial hospitalization.
Last week, the China's CCDC Weekly - modeled after the CDC's MMWR Weekly report - published the results of a retrospective investigation into this case. I've posted some excerpts, but many will want to follow the link to read the full (English) report.
I'll have a bit more on H10 spillovers after the break.
Outbreak Reports: A Retrospective Investigation of a Case of Dual Infection by Avian-Origin Influenza A (H10N5) and Seasonal Influenza A (H3N2) Viruses — Anhui Province, China, December 2023–January 2024JunHe1,2;Lei Gong3,4;Xiaolong Chen5;Deman Cheng5;Sai Hou1,3;Mengyao Kong2;Xun Wei6;Junling Yu1,3;Qian Zhu1,3;Weiwei Li1,3;Wanhang Lu1,3;Yujie Feng1,3;Hongya Gui1,3;Weixi Fang1,3;Peng Wang1,3;Yidan Xia4;Yong Sun1,3;Wanrong Luo1,3;Yun Yang5;Guowei Shen5;Hui Wang5, , ;Jiabing Wu1,3,
Summary
What is known about this topic?
H10 avian influenza viruses circulate in wild birds and can reassort with other subtypes. H10N8 and H10N3 have previously caused sporadic human infections in China.What is added by this report?
This report documents the first human case of co-infection with avian-origin H10N5 and seasonal H3N2 influenza viruses. Epidemiological investigations identified H10N5 in environmental samples linked to the patient, but no transmission to close contacts occurred.What are the implications for public health practice?
Enhanced surveillance of avian influenza in live poultry markets and poultry populations is crucial for thoroughly characterizing the epidemiology, transmission, and pathogenesis of H10N5 viruses. Strengthening assessments of outbreak control measures is essential to guide effective management.(SNIP)
DISCUSSION
The case under investigation, managed in Anhui Province from December 1 to 3, was retrospectively analyzed for this period. Epidemiologically and clinically, the patient resembled those in previous reports of human infections with H10N8 in Jiangxi Province during 2013–2014 (6–7). All patients were elderly, had pre-existing health conditions, and had either direct or indirect exposure to poultry. They exhibited a short incubation period followed by rapid disease progression. Importantly, no transmission to close contacts was observed in these cases (8–9).
Comparing H10N8 to H10N3 infections, similarities include exposure to live poultry and symptoms such as cough, fever, and chest CT imaging showing patchy high-density shadows. Elevated levels of C-reactive protein, lactate dehydrogenase, and D-dimer were also common (8,10). Both H10N5, H10N3, and H10N8 infections can lead to severe pneumonia and Type I respiratory failure (11). However, unlike H10N5, H10N3 can infect healthy young individuals and is associated with leukopenia (8,10).
Investigations identified H10N5 nucleic acid fragments in households associated with cases, mobile vendors, and live duck wholesale facilities. Retrospective inquiries, however, found no evidence of H10N5 in the original sources of the live ducks, suggesting that the virus might have been introduced or transmitted at later stages. Sequence analysis of the H10N5 subtype of the avian influenza A virus revealed that the HA segment belongs to the American lineage, while the NA segment originates from the Eurasian lineage.
The spread of H10 viruses is closely linked to wild bird migration (12); these viruses, due to their low pathogenicity and absence of noticeable symptoms, can continuously replicate within bird populations, increasing the likelihood of viral mutations and complex reassortment events (13). Previous studies have demonstrated that in southern China, domestic ducks serve as a crucial intermediary between migratory waterfowl and terrestrial poultry (14–16), thus playing a key role in inter-subtype interactions among influenza viruses (17).
Given that this is the first recorded case of H10N5 infecting humans, there is limited understanding of its infection mechanism, and follow-up cases are scarcely documented. Previous studies have indicated that after multiple passages in mice, the H10N5 virus exhibits increased virulence and mutations in its PB2 and HA proteins, suggesting a significant risk to human health (12). The H10N5 avian influenza virus shares exposure patterns, epidemiological characteristics, and clinical manifestations with other avian influenza viruses that infect humans, such as H5N8 and H10N3.
Currently, there is no evidence of human-to-human transmission. Sequence analyses and local trace-back results imply that the likelihood of the virus originating locally is minimal, with speculation pointing to long-distance transmission from wild birds.
The first known human H10 infections go back 20 years (see Avian Influenza Virus A (H10N7) Circulating among Humans in Egypt), which was followed in 2012 by a limited outbreak among workers at a chicken farm in Australia (see in EID Journal: Human Infection With H10N7 Avian Influenza).
Most of these avian flu infections were mild or asymptomatic, often only producing conjunctivitis or mild flu-like symptoms.
But in late 2013 a new H10N8 virus emerged in Mainland China infecting three people, killing at least two (see Lancet: Clinical & Epidemiological Characteristics Of A Fatal H10N8 Case).
The following year, in SwAM: European Seal Deaths Continue From H10N7 Flu, we saw estimates of more than 3,000 seals killed by avian H10N7 in Northern Europe. In 2016, in PLoS One: Pathology Of A/H10N7 In Harbor Seals, we saw evidence that ferrets were susceptible to infection, raising concerns over its zoonotic potential
In June of 2021 (see CHINA NHC Reports 1st Human H10N3 Avian Flu Infection - Jiangsu Province) China's National Health Commission made a very brief announcement on the first known human infection with avian H10N3. In that case, notification occurred just over a month after the patient was admitted to the hospital (April 28th, 2021).
In 2022, we saw a A Cryptic Report of A 2nd H10N3 Case from Hong Kong's CHP, which was further described in in 2023 in Second Identified Human Infection With the Avian Influenza Virus H10N3: A Case Report.
Five months ago, in The Lancet Microbe: Novel H10N3 Avian Influenza Viruses - a Potential Threat to Public Health, we looked at a report which identified at least 15 genotypes - all with internal genes derived from the H9N2 virus - multiple AA mammalian adaptations - and a high binding affinity to α2,6 receptor cells, which are abundant in the human upper respiratory system.
And in April of this year we saw Nature Portfolio: Preprint Case Report On China's 3rd H10N3 Case (Yunnan Province), where we learned of yet another case; this time identified as carrying HA-Q226L, PB2-D701N, PA-S409N, and M2-S31N mutations.
With at least 3 H10 subtypes (H10N8, H10N3, & H10N5) now displaying some zoonotic ability, and increasing mammalian adaptations, there are growing concerns of their future impact (see Continued Evolution of H10N3 Influenza Virus with Adaptive Mutations Poses an Increased Threat to Mammals).
Although these severe and/or fatal H10 cases remain rare, and are confined (so far) to Mainland China, H10 viruses are known to spread readily via migratory birds, and occasionally even cross oceans.
And as we've seen previously, what happens in China doesn't always stay in China.