#18,170
While H5N1 (and to a lesser extent H7 viruses) have been on our radar for more than 20 years, the number - and severity - of these avian flu threats have grown markedly over the years.
Up until 2005, when the emergence of of a new clade 2.2 at Qinghai Lake in Tibet helped to propel the virus into Europe, Africa and the Middle East, H5N1 was pretty much a regional problem for Southeast Asia.Along the way we've seen a number of `pivot' points, where the number or nature of the threat has radically changed.
For reasons not well understood, after 2007 H5N1 halted its global expansion. By 2012, the number of countries reporting HPAI had dropped from 60 to 15, and many were predicting the H5N1 threat would soon be over.
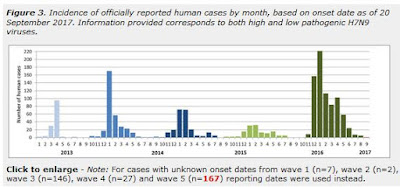
But 2013, everything changed; H7N9 emerged in China, and launched its first (of 5) seasonal epidemics, killing hundreds. Only an aggressive poultry vaccination program by China in 2017 ended that threat.
Over the next 12 months we'd also see scattered H10N8 infections reported in China, a new, and highly virulent (in poultry) HPAI H5N8 virus (clade 2.2.4.4) arrive in South Korea from China.In late 2014, HPAI H5N8 made it to North America, spread across Canada and 15 U.S. States. It was poorly suited for long-term carriage in migratory birds, however, and disappeared over the summer of 2015.
At the same time, in Egypt, H5N1 was sparking the largest outbreak in humans on record, only to pull a similar disappearing act over the summer of 2015. Exactly why it receded is still not known.
A reassorted H5N8 virus would reappear in Europe in the fall of 2016 - able to infect a much wider range of wild and migratory birds - but it too began to lose steam in 2018.
The most recent `pivot point' came in 2020, when a vastly improved H5N1 (clade 2.3.4.4b) made an abrupt return to Europe, bringing with it an increased ability to spread via migratory and wild birds, and a vastly enhanced ability to infect mammals.
With remarkable speed, HPAI H5N1 crossed the Atlantic to North America where it is now endemic, then conquered nearly all of South America, and has even encroached into Antarctica. Only Oceania, Australia, and New Zealand remain untouched, although that status could change.
The H5N1 threat we face today is far different from anything we've seen before. And it is joined by H5N6, H10Nx viruses, LPAI H9N2, and several other H5 clades, including 2.3.2.1c in Cambodia, along with a wide array of swine-origin flu viruses.
At the same time, surveillance and reporting appears to have declined, with many pandemic-weary countries holding critical information close to their vest. We often only hear about novel flu infections weeks - sometimes months - after the fact.
All of which brings us to an editorial comment in The Lancet Microbe, which describes the changing epidemiological patterns of avian influenza over the past several years, and discusses some of the challenges ahead.
I'll have a postscript after the break.
Changing epidemiological patterns in human avian influenza virus infections
Mei Kang, Hai-peng Li, Jia Tang, Xin-yu Wang, Li-fang Wang, Guy Baele et al.
Open Access Published: July 06, 2024
DOI:https://doi.org/10.1016/S2666-5247(24)00158-7Explosive geographical expansion of the avian influenza virus (AIV) continues to threaten human and animal health during and after the COVID-19 pandemic. Individuals from 17 countries across five continents have been infected by the five emerging (H5N8, H10N3, H3N8, H10N5, and H5N2) and four re-emerging (H5N1, H5N6, H7N9, and H9N2) subtypes of AIV since 2019 (appendix).
H5N1 viruses, especially those of clade 2.3.4.4b, continue to diversify genetically, spread geographically, and infect humans, as illustrated by the first ever human infection in Victoria, Australia,1 in May, 2024, and a presumed novel transmission from dairy cattle to a dairy worker from Texas, USA,2 in April, 2024. Moreover, high viral concentrations have been detected in unpasteurised milk from infected dairy cattle.
A comprehensive sequence-based analysis suggested that the viruses isolated from wild birds, cows, cats, and humans in Texas during March, 2024, share the same origin, ie, infected migratory wild birds.3 The ever-growing list of potential sources, such as alpacas,4 dairy cows, goats,2 civets,5 and minks,6 raises immense concern regarding the consequences of exposure to AIV.
In humans with AIV infection, extra-pulmonary, beyond-influenza-like conditions and symptoms at the onset of the illness, including conjunctivitis (ocular), diarrhoea (gastrointestinal), and seizures (neurological), warrant special attention.7 Reports of two fatal mixed infections in humans—one involving H10N5 and seasonal H3N2,8 and the other involving H5N1 and influenza B/Victoria lineage viruses9—suggest that mixed infections not only increase mortality risk but also reassort with human influenza viruses and potentially adapt the viruses to humans with a risk of triggering a pandemic.
Immunisation, particularly of those at high risk of exposure, is recommended to reduce the risk of coinfection of AIV and seasonal influenza viruses. In addition, educating physicians on the risk factors and natural history of human AIV infection can increase awareness and improve diagnostic ability.
Understanding the delay between illness onset and pathogen identification and hospital admission can help to tailor early risk assessment and mitigation strategies to improve prognosis and limit the spread of AIV. Compared to a 10·7-day delay during 2003–13,10 the median time-delay from illness onset to laboratory confirmation in human H5N1 cases has been reduced to 8 days since 2019 (appendix).
However, the viral identification of emerging AIVs took even longer, such as the first H10N5 human case (53 days)8 and the first H5N2 human case (35 days),11 despite the former case having a clear history of poultry exposure. The time from illness onset to admission varies among inpatients infected by H9N2, H5N1, and H5N6 viruses owing to the differences in the virus genotype, patterns in exposure, disease progression, and health-care services.
These delays have contributed to fatal outcomes among inpatients, with half of the fatal cases characterised by a delay of more than 7 days. Collecting and reporting temporal data on pathogen identification and hospital admission in a standardised manner are recommended for better risk assessment. Addressing health inequities and unmet medical needs is also necessary.
Given the unpredictable risk posed by AIVs, the implementation of One Health-based prevention and control strategies is essential. The main challenges requiring attention are disease detection and diagnosis. Although the gold standard for the diagnosis of AIV is RT-PCR testing, current resource and capacity limitations in many countries, such as issues with storing and transporting samples, restrict the amount of testing. Thus, enhanced deployment of rapid influenza diagnostic tests in both humans and animals, including neglected mammals that come in close contact with humans, is imperative.
To characterise zoonotic AIVs, viral sequencing at different outbreak stages should be encouraged to identify genetic changes that could facilitate adaptation to mammals or humans. Understanding the mechanisms that determine the host range and virulence of AIVs is essential to ensure optimal preparedness. Stricter biosecurity measures are required in all commercial farms where farm workers might be in direct contact with animals.
Furthermore, education, training, and support among farm workers might enable better self-protection and disease management. Vaccines for farmed mammals are urgently needed, particularly for species with high economic value, to reduce viral spread and economic losses and provide secondary protection to farm workers. Moreover, given the multiple detections of AIVs in produce such as uncooked meats and milk from farms susceptible to the virus, food safety measures should be strengthened. Considerable collaboration is required to address socioeconomic inequalities; overcome the limitations in access to diagnosis, treatments, and vaccines; and update strategies to combat AIVs.
The trajectory of avian flu over the past 2 decades has been far from linear, with intermittent pauses and setbacks, but it is hard to argue that we aren't facing a bigger threat today than ever before. Yet somehow our global response today seems more fragmented than it was back in 2006, when the threats were arguably fewer.
We may get away with it, of course. The next pandemic might not come for years, and it might be milder than feared; more like 2009 than 2020.
But the downsides of going unprepared into a severe pandemic can be enormous. Meaning we might not want to put too much faith in getting lucky.