# 8338
Readers with good memories will recall that in 2011, in Study: Calming The Cytokine Storm, we looked at research from The Scripps Research Institute that found a protein located on the surface of endothelial cells, called S1P1, to be largely responsible for flu-associated cytokine storms.
Rather than trying to combat the specific virus – which has a nasty habit of evolving resistance to antivirals – Scripps researchers were looking at ways of reducing the body’s sometimes excessive immune response to viral infection known as a Cytokine Storm.
Cytokines are a category of signaling molecules that are used extensively in cellular communication. They are often released by immune cells that have encountered a pathogen, and are designed to alert and activate other immune cells to join in the fight against the invading pathogen.
This cascade of immune cells rushing to the infection, if it races out of control, can literally kill the patient. Their lungs can fill with fluid (which makes a terrific medium for a bacterial co-infection), and cells in the lungs (Type 1 & Type II Pneumocytes) can sustain severe damage.
Previously, in Swine Flu Sequelae and Cytokine Storm Warnings, we looked at some of the severe lung damage during the 2009 pandemic that was thought to be due to this overreaction of the immune system.
More recently, we looked at a study by Professor Peter Doherty (see PNAS: Genetic Marker & Cytokine Levels Linked To Severity Of Human H7N9 Infection) that linked a specific genetic marker; IFITM3 CC gene variant (aka C/C Genotype) to hypercytokinemia (aka a `Cytokine Storm’), and a severe outcome, in H7N9 infections.
This genetic marker– while comparatively rare in Caucasians - is far more common in Han Chinese, and may (partially) account for some of the particularly high mortality rates we’ve seen with novel influenza’s in Asia.
Last month, China’s CDC made specific mention of the role of excess cytokine production in H7N9 infection (see NHFPC: H7N9 Avian Flu Guidance Update) where they warn: H7N9 avian influenza virus after infection the human body, can induce cytokine storm, leading to systemic inflammation, may appear ARDS, shock and multiple organ failure.
Traditionally, ARDS (Acute Respiratory Distress Syndrome) patients end up on mechanical ventilation in ICUs, and are treated with a variety of pharmacological agents to reduce infection (antibiotics) and lung inflammation (corticosteroids, Nitric Oxide, etc.).
The use of high dose corticosteroids – while fairly common with SARS and and early H5N1 cases – has been discouraged by the WHO and other health agencies due to poor long-term survival rates.
Hence the need for a better tolerated, more effective, and targeted drug regimen against the cytokine storm.
All of which serves as prelude to a new report from the The Scripps Research Institute updating their search for a drug to modulate the body’s immune response, and mapping the cytokine signaling and production process. Their findings appear this week in the early edition of the journal PNAS.
Mapping the innate signaling cascade essential for cytokine storm during influenza virus infection
John R. Teijaroa, Kevin B. Walsha,1, Stephanie Ricea, Hugh Rosenb,c,2, and Michael B. A. Oldstonea,2
Significance
Cytokine storm plays an essential and commanding role in the clinical outcome and pathogenesis of influenza virus infection. We previously documented that a small molecule that activates sphingosine-1-phosphate-1 receptor (S1P1R) signaling is primarily responsible for blunting cytokine storm to protect the infected host from the consequences of influenza infection. In the present study, we map host innate signaling pathways of cytokine storm and chart where along those pathways the drug is effective. We find that the efficacy of S1P1R agonist in blunting cytokine storm is through global inhibition downstream of myeloid differentiation primary response gene 88 and IFN-β promoter stimulator-1 signaling.
Although the bulk of this study is behind a pay wall, we get a pretty detailed overview from the following press release from the Scripps Institute.
News Release
LA JOLLA, CA—February 27, 2014—Scientists at The Scripps Research Institute (TSRI) have mapped key elements of a severe immune overreaction—a “cytokine storm”—that can both sicken and kill patients who are infected with certain strains of flu virus.
Their findings, published in this week’s online Early Edition of the Proceedings of the National Academy of Sciences, also clarify the workings of a potent new class of anti-inflammatory compounds that prevent this immune overreaction in animal models.
“We show that with this type of drug, we can quiet the storm enough to interfere with the virus-induced disease and lung injury, while still allowing the infected host to mount a sufficient immune response to eliminate the virus,” said John R. Teijaro, an assistant professor in TSRI’s Department of Immunology and Microbial Science and first author of the study.
“This study provides insights into mechanisms that are chemically tractable and can modulate these cytokine storms,” said Hugh Rosen, professor in TSRI’s Department of Chemical Physiology and senior author of the study with Michael B. A. Oldstone, professor in TSRI’s Department of Immunology and Microbial Science.
Calming the Storm
A cytokine storm is an overproduction of immune cells and their activating compounds (cytokines), which, in a flu infection, is often associated with a surge of activated immune cells into the lungs. The resulting lung inflammation and fluid buildup can lead to respiratory distress and can be contaminated by a secondary bacterial pneumonia—often enhancing the mortality in patients.
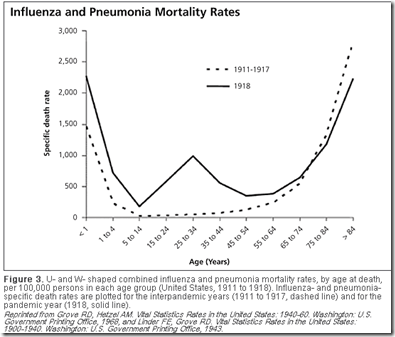
This little-understood phenomenon is thought to occur in at least several types of infections and autoimmune conditions, but it appears to be particularly relevant in outbreaks of new flu variants. Cytokine storm is now seen as a likely major cause of mortality in the 1918-20 “Spanish flu”—which killed more than 50 million people worldwide—and the H1N1 “swine flu” and H5N1 “bird flu” of recent years. In these epidemics, the patients most likely to die were relatively young adults with apparently strong immune reactions to the infection—whereas ordinary seasonal flu epidemics disproportionately affect the very young and the elderly.
For the past eight years, Rosen’s and Oldstone’s laboratories have collaborated in analyzing the cytokine storm and finding treatments for it. In 2011, led by Teijaro, who was then a research associate in the Oldstone Lab, the TSRI team identified endothelial cells lining blood vessels in the lungs as the central orchestrators of the cytokine storm and immune cell infiltration during H1N1 flu infection.
In a separate study, the TSRI researchers found that they could quiet this harmful reaction in flu-infected mice and ferrets by using a candidate drug compound to activate immune-damping receptors (S1P1 receptors) on the same endothelial cells. This prevented most of the usual mortality from H1N1 infection—and did so much more effectively than the existing antiviral drug oseltamivir, although the combination of both therapies worked even better. “That was really the first demonstration that inhibiting the cytokine storm is protective,” said Teijaro.
This press release goes on to state that the experimental drug – CYM5442 – is now being tested in clinical trials, with uses that extend far beyond just influenza-related ARDS.
An optimized version of CYM5442, initially developed by Rosen and fellow TSRI chemist Ed Roberts, has been licensed to the pharmaceutical company Receptos. It is now in Phase 3 clinical trials for treating relapsing-remitting multiple sclerosis and Phase 2 trials for ulcerative colitis. Other S1P1 receptor agonists are in development for inflammatory conditions. A less-specific S1P receptor agonist—which hits S1P1, but also hits S1P3, S1P4 and S1P5, with potential off-target effects—is already approved for treating multiple sclerosis.
While it is hard to find anything `good’ to say about the emergence of novel viral threats over the past dozen years (H5N1, SARS, H7N9, etc.), it has prompted a remarkable amount of research – not only into the pathogens themselves - but into the complex and far from completely understood inner workings of our own immune system.
Research that has the potential to pay health benefits far beyond simply treating viral infections.