# 6990
Over the past couple of years we’ve examined several studies looking at the seasonality of influenza – both in temperate and tropical climes – the most recent being earlier this week in PLoS One: High Humidity Reduces Flu’s Infectivity.
In that study researchers tested the viability of influenza viruses at various relative humidity (RH) levels between 7% and 73%. Infectivity was assessed by the viral plaque assay.
They found that above 40% RH, infectivity dropped sharply.
Which fits nicely with the yearly increase of influenza across temperate zones during the winter, when RH is often 75% lower than during the summer months.
But it does little to explain the year-round transmission of influenza in tropical climes.
Last December, we took a run at another study (see Influenza Virus Survival At Opposite Ends Of The Humidity Spectrum) conducted by researchers from Virginia Tech – that looked at a much broader range of humidity levels (up to 100%).
They found both extremely low and extremely high humidity humidity appeared to aid and abet the viability of the flu virus – at least when it resides in mucus and respiratory fluids like those found in your nose, throat, or lungs.
Essentially, these researchers inoculated droplets of simulated respiratory fluids (containing salts & proteins) with influenza viruses, and tested their survivability at different humidity levels.
- At low humidity (< 50%) the droplets evaporated quickly, and the virus survived well in a dry environment.
- At high humidity (near 100%), the droplets were stable, and the virus survived as well.
But at humidity levels in-between, the droplets slowly dried out, increasing the concentration of salts and proteins to which the viruses were exposed, decreasing their survival rate.
These studies suggest that there is a `sweet spot’ in RH (approx 40%-95%) where flu viruses have difficulty surviving. At levels above or below, the virus fares much better.
This would help explain why influenza is primarily a winter event in temperate zones, but can still transmit in the exceptionally humid tropics year-round.
In 2008 researchers Jeffrey Shaman and Melvin Kohn established a correlation between the AH (Absolute Humidity) and the survival, and transmission of the influenza virus (see It's Not So Much The Heat, It's The Humidity).
Absolute humidity modulates influenza survival, transmission, and seasonality
Jeffrey Shaman, and Melvin Kohn
In 2010, Jeffrey Shaman returned with Virginia E. Pitzer, Cécile Viboud, Bryan T. Grenfell and Marc Lipsitch – and penned a study in PLoS Biology called:
Absolute Humidity and the Seasonal Onset of Influenza in the Continental United States
(Excerpt)
Here we extend these findings to the human population level, showing that the onset of increased wintertime influenza-related mortality in the United States is associated with anomalously low absolute humidity levels during the prior weeks. We then use an epidemiological model, in which observed absolute humidity conditions temper influenza transmission rates, to successfully simulate the seasonal cycle of observed influenza-related mortality.
Shaman and Viboud et al. return today with a new NIH/Fogarty study appearing in PloS Pathogens that finds it is both cold-dry and humid-rainy conditions that can exacerbate influenza outbreaks.
A finding that fits rather nicely with the Virginia Tech research mentioned above.
Environmental Predictors of Seasonal Influenza Epidemics across Temperate and Tropical Climates
James D. Tamerius, Jeffrey Shaman, Wladmir J. Alonso, Kimberly Bloom-Feshbach, Christopher K. Uejio, Andrew Comrie, Cécile Viboud
Abstract (reparagraphed for readability)
Human influenza infections exhibit a strong seasonal cycle in temperate regions. Recent laboratory and epidemiological evidence suggests that low specific humidity conditions facilitate the airborne survival and transmission of the influenza virus in temperate regions, resulting in annual winter epidemics. However, this relationship is unlikely to account for the epidemiology of influenza in tropical and subtropical regions where epidemics often occur during the rainy season or transmit year-round without a well-defined season.
We assessed the role of specific humidity and other local climatic variables on influenza virus seasonality by modeling epidemiological and climatic information from 78 study sites sampled globally.
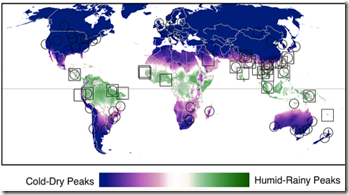
We substantiated that there are two types of environmental conditions associated with seasonal influenza epidemics: “cold-dry” and “humid-rainy”.
For sites where monthly average specific humidity or temperature decreases below thresholds of approximately 11–12 g/kg and 18–21°C during the year, influenza activity peaks during the cold-dry season (i.e., winter) when specific humidity and temperature are at minimal levels. For sites where specific humidity and temperature do not decrease below these thresholds, seasonal influenza activity is more likely to peak in months when average precipitation totals are maximal and greater than 150 mm per month.
These findings provide a simple climate-based model rooted in empirical data that accounts for the diversity of seasonal influenza patterns observed across temperate, subtropical and tropical climates.
For more, we have a press release from the NIH/Fogarty International Center.
NIH study sheds light on role of climate in influenza transmission
Two types of environmental conditions—cold-dry and humid-rainy—are associated with seasonal influenza epidemics, according to an epidemiological study led by researchers at the National Institutes of Health's Fogarty International Center. The paper, published in PLOS Pathogens, presents a simple climate-based model that maps influenza activity globally and accounts for the diverse range of seasonal patterns observed across temperate, subtropical and tropical regions.
The findings could be used to improve existing current influenza transmission models, and could help target surveillance efforts and optimize the timing of seasonal vaccine delivery, according to Fogarty researcher Cecile Viboud, Ph.D., who headed the study. "The model could have a broader application, encouraging researchers to analyze the association between climatic patterns and infectious disease across a wide range of diseases and latitudes," said Viboud.
Human influenza infections exhibit a strong seasonal cycle in temperate regions, and laboratory experiments suggest that low specific humidity facilitates the airborne survival and transmission of the virus in temperate regions. Specific humidity is the ratio of water vapor to dry air in a particular body of air while relative humidity—commonly used in weather forecasts—is the amount of water vapor in the air relative to its capacity to hold water vapor, and is primarily a function of temperature.
Data from animal studies indicate low temperature and humidity increase the duration of the virus's reproduction and expulsion in infected organisms and virus stability in the environment, increasing the probability of transmission through coughing, sneezing or breathing. In contrast, high temperature seems to block airborne transmission.
While climatic conditions appear to play a big role in the infectivity of influenza, it is by no means the only factor. Again, from the press release:
"Further work should focus on examining the role of population travel and other factors in influenza transmission," notes Mark Miller, M.D., director of Fogarty's Division of International Epidemiology and Population Studies. "
Understanding the climatic conditions under which influenza (and perhaps other) viruses transmit best may provide us with an improved ability to forecast regional outbreaks.
But perhaps as importantly, this knowledge may also show us how to adjust indoor environments to curb flu transmission. The upshot from the NIOSH report from earlier this week (see press release Higher indoor humidity inactivates flu virus particles) reads:
The study concludes that maintaining indoor relative humidity at levels greater than 40% can significantly reduce the infectious capacity of aerosolized flu virus.
Something that environmental managers at hospitals, office buildings, schools, and other locations may want to take notice of before we enter the next influenza epidemic.