Photo Credit – Wikipedia
# 5683
Over the past couple of months Hong Kong has experienced an unusually large outbreak of Scarlet Fever caused by the bacterium Streptococcus pyogenes; some strains of which have reportedly `mutated’, picking up greater transmissibility and increased antibiotic resistance.
For earlier reports see here, here, and here.
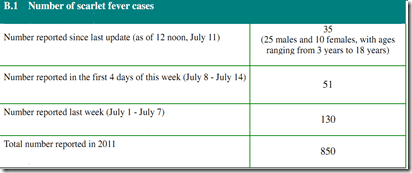
The latest report from the Centre for Health Protection lists 35 new cases over the 72-hour weekend reporting period; an increase of 113 over a week ago.
But S. pyogenes may be the cause of a number of different disease processes, among them pharyngitis ("strep throat"), scarlet Fever, localized skin infections ("impetigo"), and even deep tissue infections resulting in necrotizing fasciitis.
Infection with certain strains of S. pyogenes can lead to the release of bacterial toxins, and in rare cases can result in Toxic Shock Syndrome.
Yesterday the CHP released the following brief announcement of a Group A Strep-related pediatric TSS (Toxic Shock Syndrome) case.
10 July 2011
A paediatric case of Group A Streptococcal Toxic Shock Syndrome
The Centre for Health Protection (CHP) of the Department of Health today (July 10) is investigating a critical case of Group A Streptococcal infection involving a 10-year-old boy with chronic illness.
The patient presented with fever and vomiting and attended the Accident and Emergency Department (AED) of Pok Oi Hospital (POH) on July 8. The clinical diagnosis was gastroenteritis. No hospitalization is required.
His condition however deteriorated with cough and shortness of breath the next day. He reattended AED of POH, and was transferred to Tuen Mun Hospital for management.
His condition further deteriorated and he developed toxic shock syndrome. He is now in critical condition.
Culture of his gastric lavage grew Group A Streptococcus.
The boy had no recent travel history. His home contacts were asymptomatic.
CHP’s investigation continued.
Ends/Sunday, July 10 2011
According to this report in the Hong Kong Standard, government authorities state that this case "is not related to scarlet fever".
While the type of infection isn’t characterized in the CHP report, the child is referred to has having `chronic illness’, which can sometimes be a factor in developing an invasive Strep infection.
Also unknown at this time is whether child’s infection is due to one of the antibiotic-resistant strains currently being seen in the scarlet fever outbreak.
The CDC describes Streptococcal Toxic Shock Syndrome (STSS) this way.
Streptococcal toxic shock syndrome (STSS), causes blood pressure to drop rapidly and organs (e.g., kidney, liver, lungs) to fail. STSS is not the same as the "toxic shock syndrome" frequently associated with tampon usage. About 20% of patients with necrotizing fasciitis and more than half with STSS die. About 10%-15% of patients with other forms of invasive group A streptococcal disease die.
The Toxic Shock Syndrome associated with Tampon use in the early 1980s was caused by Staphylococcus aureus, not Streptococcus pyogenes.
Lastly, the CDC has some advice on how to prevent the spread of Group A Strep bacteria:
What can be done to help prevent group A streptococcal infections?
The spread of all types of GAS infection can be reduced by good hand washing, especially after coughing and sneezing and before preparing foods or eating. Persons with sore throats should be seen by a doctor who can perform tests to find out whether the illness is strep throat. If the test result shows strep throat, the person should stay home from work, school, or day care until 24 hours after taking an antibiotic.
All wounds should be kept clean and watched for possible signs of infection such as redness, swelling, drainage, and pain at the wound site. A person with signs of an infected wound, especially if fever occurs, should immediately seek medical care.
It is not necessary for all persons exposed to someone with an invasive group A strep infection (i.e. necrotizing fasciitis or strep toxic shock syndrome) to receive antibiotic therapy to prevent infection. However, in certain circumstances, antibiotic therapy may be appropriate. That decision should be made after consulting with your doctor.