Group A streptococcal infections: update on seasonal activity, 2014 to 2015
Ref: HPR 9(5)
# 9717
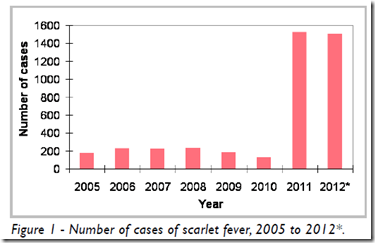
In 2014 the UK saw a huge increase in the number of Scarlet Fever cases (blue line in chart above), after a decade of declining or flat numbers. We looked at that rising tide of cases last March in UK : Sharp Rise In Scarlet Fever Cases In 2014, but the peak in cases didn’t occur until April.
Before the year ended, more than 14,000 Scarlet fever cases were diagnosed in the UK, the highest number since the 1960s.
Once again this year Scarlet Fever notifications are up, averaging more than 200 cases a week for the past 6 weeks (n=1265). As the chart above shows (red line), the number of cases is running nearly double that of last year, with the expected peak of the season still weeks (or months) away.
Scarlet Fever primarily affects children under the age of 12. It is highly contagious, there is no vaccine, but antibiotics are generally effective when treated early.
Scarlet fever (Group A Streptococcus or GAS) is caused by the bacterium Streptococcus pyogenes - which like viruses, can evolve over time – sometimes resulting in increased virulence, greater transmissibility, and/or antibiotic resistance.
Strains are identified by changes in their M-protein gene sequence (emm types) – which often determines virulence - and within these types new variants can emerge.
Although less common, a more serious yet related illness is called iGAS (invasive Group A Strep), which indicates infection of the bloodstream, deep tissues, or lungs, and may result in severe (and frequently fatal) cases of necrotizing fasciitis and streptococcal toxic shock syndrome.
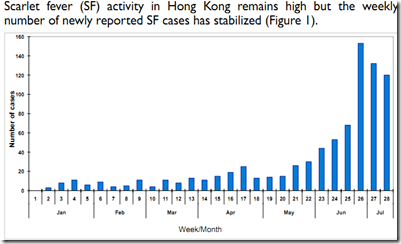
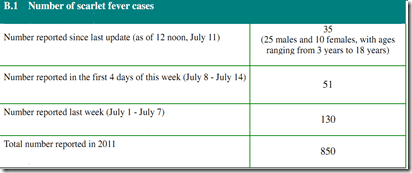
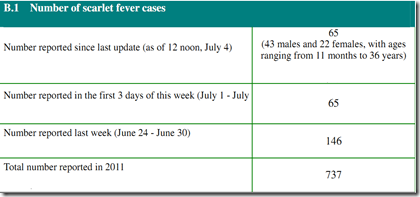
In 2011 and 2012 we followed an unusual erythromycin resistant (but still sensitive to Penicillin & other 1st generation cephalosporins) scarlet fever outbreak in Hong Kong (see Hong Kong: Scarlet Fever In 2012), which resulted in a small number of pediatric fatalities.
Last November a Nature Genetics journal article attributed Hong Kong’s severe outbreak to the emergence of a new emm12 variant (see Emergence of scarlet fever Streptococcus pyogenes emm12 clones in Hong Kong is associated with toxin acquisition and multidrug resistance).
On Friday the UK’s PHE released the following statement about this year’s increased activity:
Scarlet fever notifications continue to increase
From: Public Health England
First published: 13 February 2015
Latest PHE report shows a high number of scarlet fever notifications across England, with 1265 new cases reported in the first 6 weeks of 2015.
Steep increases in scarlet fever activity are being seen across the country, with over 300 cases reported last week (2 to 9 February 2015).
Increases in scarlet fever are normal at this time of year as we approach high season between March and April. However, the numbers of cases currently being reported are above what is typical for this time of the year. Whilst this might reflect heightened awareness and improved diagnosis and/or notification practices, the high number of cases currently being notified are of concern. Last year in England, over 14,000 cases of scarlet fever were notified, the highest total since the late 1960s.
Dr Theresa Lamagni, PHE’s head of streptococcal infection surveillance, said:
As we enter into high season for scarlet fever, we ask GPs and other frontline medical staff to be mindful of the current high levels of scarlet fever activity when assessing patients. Prompt notification of cases to local health protection teams is critical to enable local monitoring and rapid response to outbreaks. Schools and nurseries should similarly be mindful of the current elevated levels of scarlet fever and promptly inform local health protection teams at an early stage if they become aware of cases, especially if more than 1 child is affected.
In March of 2014, during last year’s dramatic spike in cases, the Eurosurveillance Journal ran a Rapid Communications Report that described the UK outbreak, and discussed possible causes for the recent increase in cases.
Eurosurveillance, Volume 19, Issue 12, 27 March 2014
Rapid communications
Increase in scarlet fever notifications in the United Kingdom, 2013/2014
R Guy1, C Williams2, N Irvine3, A Reynolds4, J Coelho1, V Saliba1, D Thomas2, L Doherty3, V Chalker1, B von Wissmann4, M Chand1, A Efstratiou1, M Ramsay1, T Lamagni (
)1
<SNIP>
Discussion
Scarlet fever incidence has shown a remarkable increase this season. Previous analysis of scarlet fever notifications in England over the last century suggest cyclical patterns of incidence, with resurgences occurring on average every four years [3]. The last peak year for scarlet fever was 2008/09, with incidence of invasive disease tending to mirror those of superficial manifestations of GAS infection in many but not all years [4]. While the enhanced media coverage and public health alerts may have increased case ascertainment during this season, the escalation prior to this suggests a genuine increase in disease incidence. The reasons behind this increase are unclear but may be attributable to a natural cycle in disease incidence.
It remains possible that the increase or part of the increase is attributable to changes in virulence of circulating strains or increased incidence in particular risk groups. An exceptional increase in scarlet fever incidence in Hong Kong during 2011 and 2012 was attributed to the introduction of a new emm12 strain [5]. Continued vigilance for the emergence of a novel strain or changes in pattern of clinical disease is essential.
At present, antimicrobial susceptibility results are not indicating any change in antibiotic susceptibility [6]. Analysis of isolates originating from normally sterile sites, which were submitted to the national reference laboratory, has not identified any unusual types circulating, although a slight increase in the proportion of due to emm3 is currently being observed. Strains harbouring this emm type were implicated in the UK rise in incidence in scarlet fever and iGAS infection during 2008/09 [7], and also implicated in population increases in iGAS infection incidence in Ireland in 2013 [8]. While the current rise in emm3 is slight, it raises some concern given its association with a higher case fatality rate than other emm types [9;10]. Rapid assessment of changes in case fatality rate will assist in monitoring any such changes during the current season.
As a result of the current rise in scarlet fever notifications, clinicians, microbiologists and health protection specialists across Europe should continue to be mindful of potential increases in invasive disease and maintain a high index of suspicion in relevant patients, as early recognition and prompt initiation of specific and supportive therapy for patients with iGAS infection can be life-saving. Alerts have been issued by local health protection staff to frontline medical staff in the UK. An unusual pattern of outbreaks of scarlet fever has also been noted in Belgium during this season (K Loens, personal communication, March 2014). Comparison of strains across the two countries would be beneficial in understanding the current situation in the UK.
I’ll update this story later in the spring, as the size of this year’s outbreak becomes more apparent.