#12,420
While it rarely gets star billing - LPAI H9N2 - ubiquitous in Asian poultry, yet only rarely found infecting humans, is nonetheless an important player in the avian flu world.
It is considered to have some pandemic potential of its own, but by far its greatest contribution to date has been to to lend some of its internal genes to recently emerged HPAI & LPAI viruses, including H5N8, H5N6, and H7N9 (see graphic below).
 |
| H7N9 Genetic Structure - Credit Eurosurveillance |
H9N2's contributions to the creation of these novel HPAI/LPAI strains is not a one shot deal.
In 2014's Eurosurveillance:The Evolving Threat From New, Reassorted H7N9 Viruses, researchers reported finding ongoing and `dynamic reassortments between influenza A(H7N9) and A(H9N2) viruses since the outbreak of A(H7N9) virus infection in March 2013.'
This continual participation in the evolution of H7N9 (and other) avian viruses has led to the creation of new lineages, and dozens of new genotypes, a pattern that makes identifying any changes in H9N2's genetic structure and behavior all the more important.
In early 2014 The Lancet carried a report entitled Poultry carrying H9N2 act as incubators for novel human avian influenza viruses where researchers warned that `reassortment between the prevalent poultry H9N2 viruses (providing genetic segments) and the influenza virus from wild birds could make the influenza evolve to adapt to domestic hosts.'
Eighteen months ago, in PLoS Path: Genetics, Receptor Binding, and Transmissibility Of Avian H9N2 researchers found evidence of Chinese H9N2 viruses binding preferentially to alpha 2,6 receptor cells - the type commonly found in the human upper respiratory tract - rather than to alpha 2,3 receptor cells which are found in the gastrointestinal tract of birds.
As we've seen with other widely distributed avian flu viruses, H9N2 has evolved into many different lineages and/or genotypes.The virus you get in Bangladesh is quite distinct from the version you’ll find in China, the Middle East, or . . . in Korea.All of which serves as prelude to a new study appearing in Veterinary Microbiology which looks at the genetic evolution, and behavior, of H9N2 viruses collected in South Korea.
Their findings suggest the South Korean lineage of H9N2 may be making strides towards better mammalian adaptation, something which could have serious implications - not only for H9N2 as a standalone pandemic threat - but also conceivably for those viruses it lends its genes to in the future.
First, the link and abstract to the study, then I'll return with a bit more.
Genetics and biological property analysis of Korea lineage of influenza A H9N2 viruses
Min Kang, Hyung-Kwan Jang,
https://doi.org/10.1016/j.vetmic.2017.04.014
Highlights
• Little information is available about the biological properties of H9N2 viruses of Y439 lineage in mammals.
• Some Korean H9N2 viruses caused higher than expected mortalities to mice without prior adaptation.
• Korean H9N2 with mammalian host-tropic mutations caused higher than expected mortalities to mice without prior adaptation.
• H9N2 viruses with enhanced pathogenicity to mice might have been established recently from endemic viruses.
Abstract
H9N2 influenza viruses have been detected from wild and domestic avian species including chickens and ducks worldwide. Few studies have compared the biological properties of different H9N2 lineages or determined whether certain lineages might pose a higher risk to mammals, especially H9N2 viruses of Korean lineage.
The objective of this study was to characterize the genetic and biological properties of 22 Korean H9N2 viruses and assess their potential risks to mammals. Their complete genomes were analyzed.
Some Korean H9N2 viruses were found to carry mammalian host-specific mutations.
Based on genomic diversities, these H9N2 viruses were divided into 12 genotypes. All 22 showed preferential binding to human-like receptor. Two of eight H9N2 viruses were highly lethal to mice, causing 90–100% mortality without prior adaptation and severe respiratory syndromes associated with diffuse lung injury, severe pneumonia, and alveolar damage.
These findings suggest that recent Korean H9N2 viruses might have established a stable sublineage with enhanced pathogenicity to mice. Various H9N2 strains pathogenic to mice were endemic in wild bird, poultry farm, and live bird markets, suggesting that Korean H9N2 viruses could evolve to become a threat to humans.
The findings emphasize the necessity of careful, continuous, and thorough surveillance paired with risk-assessment for circulating H9N2 influenza viruses.
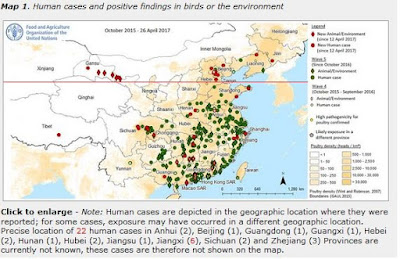
In the 16 years between 1998 and the end of 2014, the WHO had been notified of just 18 cases globally (see FluTrackers Global Cumulative H9N2 Partial Case List 1998-2016). Over the last 28 months, however, the WHO has been notified of 20 new cases (14 in China, 4 in Egypt, and 2 in Bangladesh).
All of which raises the question. Are we just getting better at detecting human infections, or is the virus getting better at infecting humans?While this increased surveillance could easily explain this jump in cases, the virus continues to evolve and show signs of becoming a more mammalian adapted virus.
Which means we ignore this meddlesome virus at our own peril.